Is it normal that antibiotics give my child diarrhea?
As the main tool in the fight against bacterial infections, antibiotics save lives. However, in destroying the species that cause the infections, they also eradicate the good bacteria in our bodies, known as the microbiota, and can cause side effects especially in our gut flora.1
So, is it normal that antibiotics give your child diarrhea? Answer below!
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Diarrhea can affect up to 80% of children taking antibiotic treatment.
Since the discovery of penicillin in 1928, antibiotics have been the main weapon in the fight against bacterial infections and have increased life expectancy by almost 20 years, in parallel with vaccinations.2
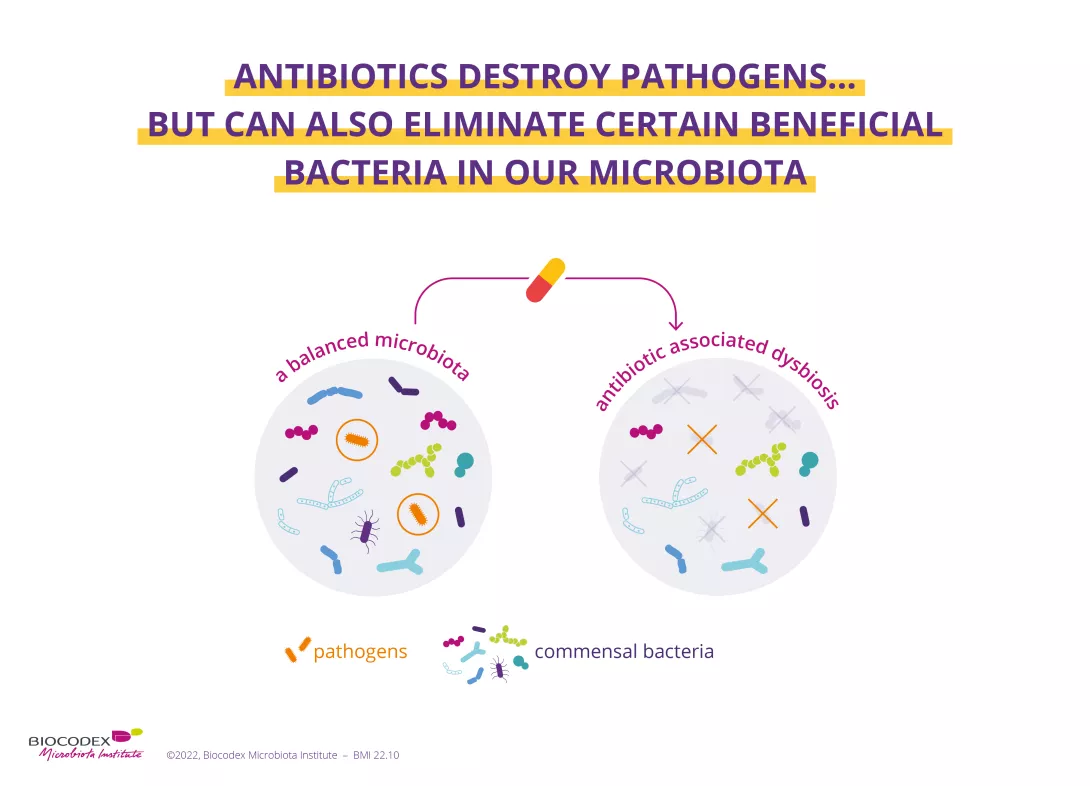
However, although antibiotics eradicate the (sidenote: Pathogen A pathogen is a microorganism that causes, or may cause, disease. Pirofski LA, Casadevall A. Q and A: What is a pathogen? A question that begs the point. BMC Biol. 2012 Jan 31;10:6. ) bacteria responsible for our infections, they can also destroy some beneficial bacteria in our microbiota causing an imbalance within this complex ecosystem, this is called (sidenote: Dysbiosis Generally defined as an alteration in the composition and function of the microbiota caused by a combination of environmental and individual-specific factors. Levy M, Kolodziejczyk AA, Thaiss CA, et al. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17(4):219-232. ) .3
Up to 35% of patients may be affected by Antibiotics-Associated Diarrhea
Up to 80% of children may be affected by Antibiotics-Associated Diarrhea
This dysbiosis can have consequences for our health, such as bowel transit changes that can lead to antibiotic-associated diarrhea (AAD):4 this is moreover the most common side effect of antibiotics in the short term.
It is usually mild and stops by itself after 1–5 days. It can affect up to 35% of patients4–6 on antibiotics but in children, this figure can reach 80%.5
Antibiotics could generate longer-term effects
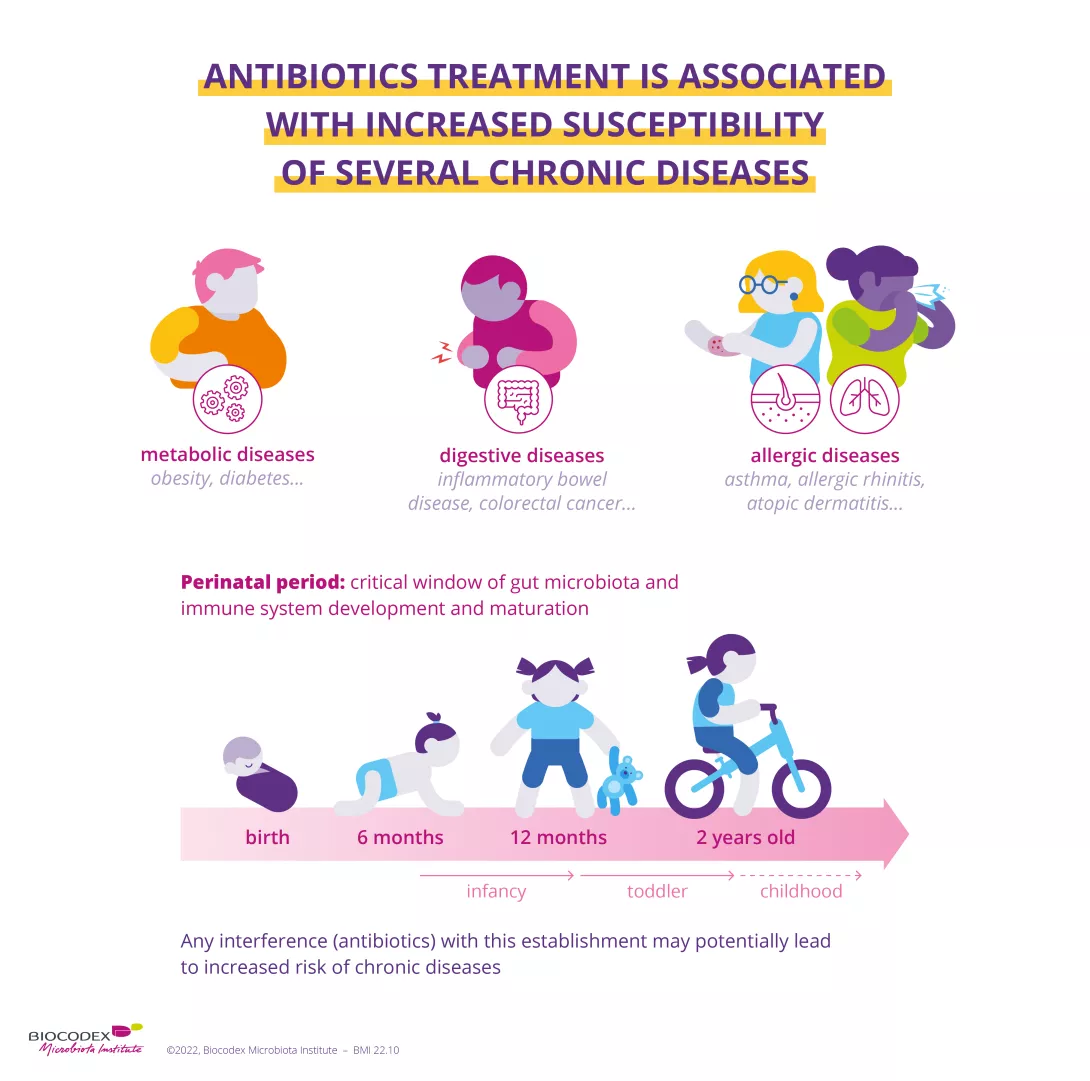
Antibiotic-associated diarrhea is not the only side effect, the dysbiosis is supposedly responsible for longer-term effects when it occurs very early in life. During the perinatal period, that is the critical time window for the development and maturation of the microbiota and of the immune system,7 disruption of the gut microbiota associated with the taking of antibiotics is suspected to increase the risk of several chronic diseases (obesity, diabetes, asthma, chronic inflammatory bowel disease).8
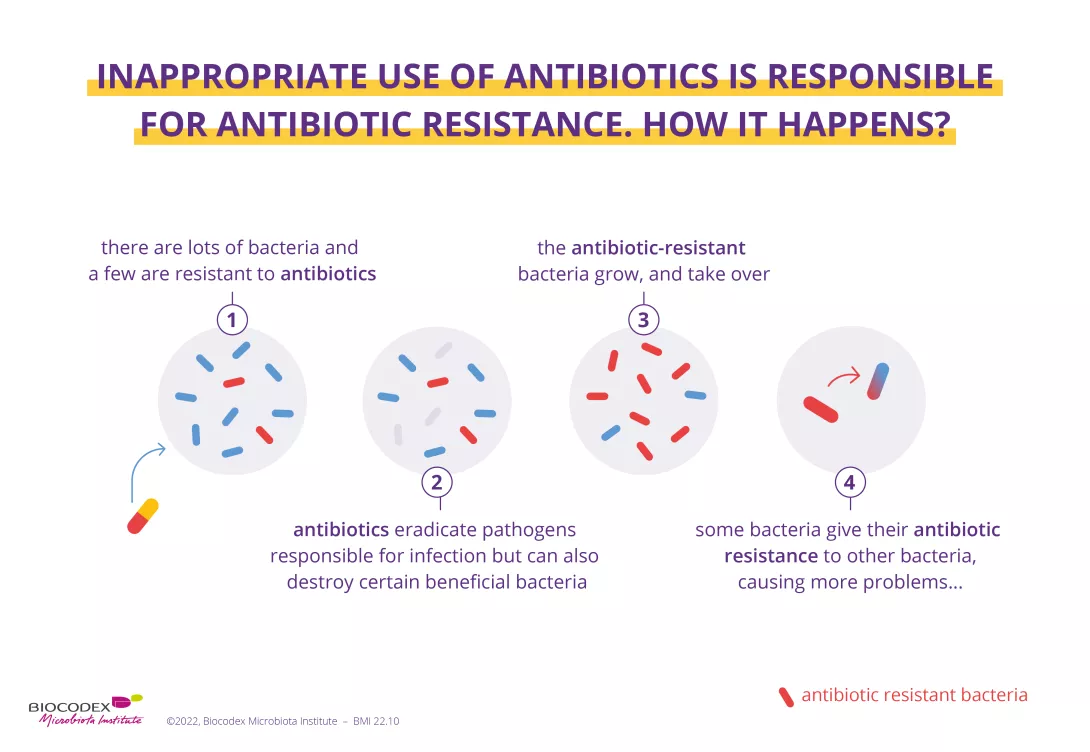
In addition, poor compliance with antibiotic treatments (excessive or inappropriate use) is responsible for antibiotic resistance,9 meaning that antibiotic treatment is no longer effective against bacterial infection. This phenomenon leads to longer hospital stays, even sometimes deaths, and rising health care costs.
Each year, from 18–24 November, the WHO holds its World AMR Awareness Week to promote the correct use of antibiotics and to encourage the general public, health professionals, and politicians to adopt best practices to combat the emergence and spread of resistance.
Gut microbiota: still many things to be discovered
Each year, since 2015, the WHO organizes the World AMR Awareness Week (WAAW), which aims to increase awareness of global antimicrobial resistance.
Antimicrobial resistance occurs when bacteria, viruses, parasites and fungi change over time and no longer respond to medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat, increasing the risk of disease spread, severe illness and death.
Held on 18-24 November, this campaign encourages the general public, healthcare professionals and decision-makers to use antibiotics, antivirals, antifungals and antiparasitics carefully, to prevent the further emergence of antimicrobial resistance.
Recommended by our community

"Thank for sharing" - Merle Creed (From My health, my microbiota)
"So true" - Clara Autowski (From My health, my microbiota)
"Safe and effective" - Dave Beal (From My health, my microbiota)
4 Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med 2002;346:334-9.
5 McFarland LV, Ozen M, Dinleyici EC et al. Comparison of pediatric and adult antibiotic-associated diarrhea and Clostridium difficile infections. World J Gastroenterol. 2016;22(11):3078-3104.
6 Theriot CM, Young VB. Interactions Between the Gastrointestinal Microbiome and Clostridium difficile. Annu Rev Microbiol. 2015;69:445-461.















