Impact of antibiotics on the gut microbiota
A major medical discovery of the 20th century, antibiotics have saved millions of lives, but their excessive and often inappropriate use has led to the emergence of multiple forms of antibiotic resistance. This past November, the WHO publicly highlighted the importance of using antibiotics prudently.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information

About this article
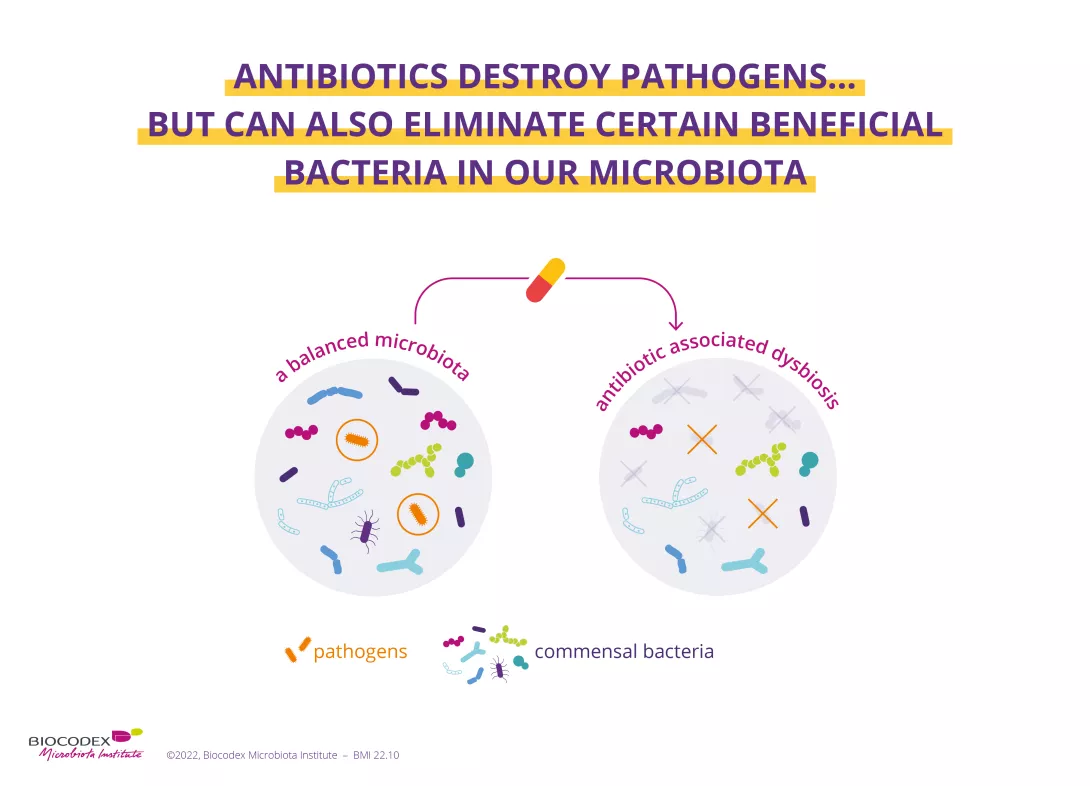
The use of antibiotics increased by 65% between 2000 and 2015. This new study reminds us that when eradicating pathogenic germs responsible for infections, antibiotics can also destroy beneficial bacteria in the gut microbiota, thereby causing an imbalance (dysbiosis) within this ecosystem, with potential short and long-term consequences.
If you are interested in the effects of antibiotics on your health and your microbiota, or if you want to know more about the World AMR Awareness Week (WAAW), we recommend that you go to this other dedicated page:
Antibiotics: what impact on the microbiota and on our health?
Adverse effects on microbiota in the short and medium term...
The first thing to note is that antibiotics disrupt the balance existing in the gut microbiota. By eliminating certain bacteria, they allow other pathogens to occupy the free space and multiply. One consequence is antibiotic-associated diarrhea, which affects between 5% and 35% of patients but usually resolves spontaneously within a few days. However, some forms of diarrhea can be more severe and when caused by Clostridioides difficile they may even be fatal.
The second observation is that antibiotics are linked to a reduction in microbiota diversity. A return to equilibrium may take some time, with certain bacteria still absent after several months. Lastly, the repeated or inappropriate use of antibiotics leads bacteria to develop strategies to circumvent their effects. Bacteria can become antibiotic-resistant, thereby rendering treatments ineffective. The experts’ predictions are unsettling: unless drastic measures are taken to address the issue, the misuse of antibiotics could cause ten million deaths worldwide by 2050.
+65% The use of antibiotics increased by 65% between 2000 and 2015.
5% - 35% Antibiotic-associated diarrhea affects between 5% and 35% of patients.
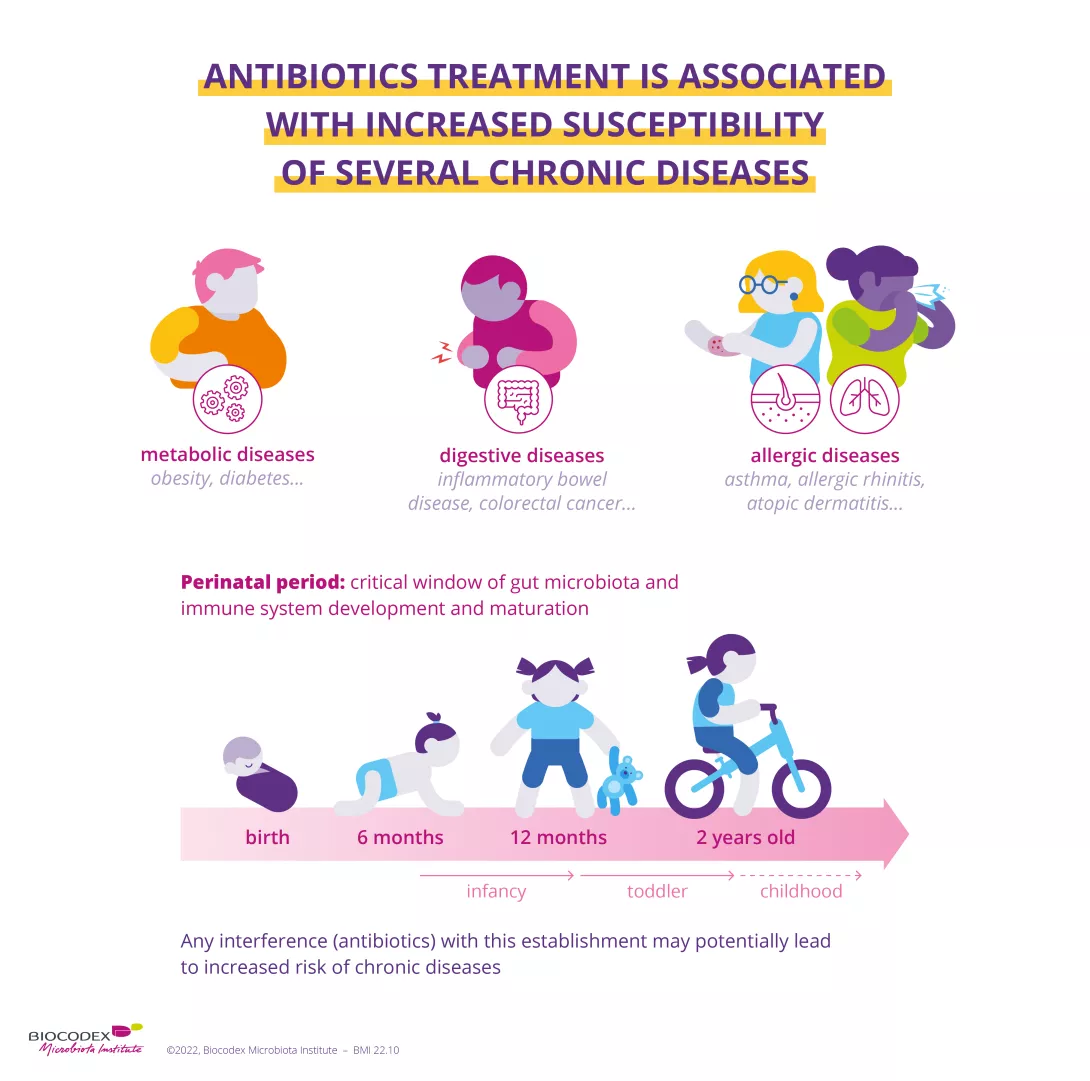
...with serious long-term consequences
Systemic use of antibiotics is still far too widespread among infants and children and is thought to be associated with the development of diseases later in life (obesity, asthma, allergies, inflammatory bowel disease). This battle is far from won and the scientific community is actively seeking new strategies to restore the gut microbiota, based on multiple modulation pathways (diet, probiotics, prebiotics).
The gut microbiota
Each year, since 2015, the WHO organizes the World AMR Awareness Week (WAAW), which aims to increase awareness of global antimicrobial resistance.
Antimicrobial resistance occurs when bacteria, viruses, parasites and fungi change over time and no longer respond to medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat, increasing the risk of disease spread, severe illness and death.
Held on 18-24 November, this campaign encourages the general public, healthcare professionals and decision-makers to use antibiotics, antivirals, antifungals and antiparasitics carefully, to prevent the further emergence of antimicrobial resistance.














