Microbiota, asthma and antibiotics: it’s all in the nose!
We know that infants exposed to antibiotics are more likely to develop asthma at a later stage in life but science still struggles to explain the mechanisms behind this correlation. One clue seems to be right under our nose, or rather inside it! The nasal microbiota appears to play a central role.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information

About this article
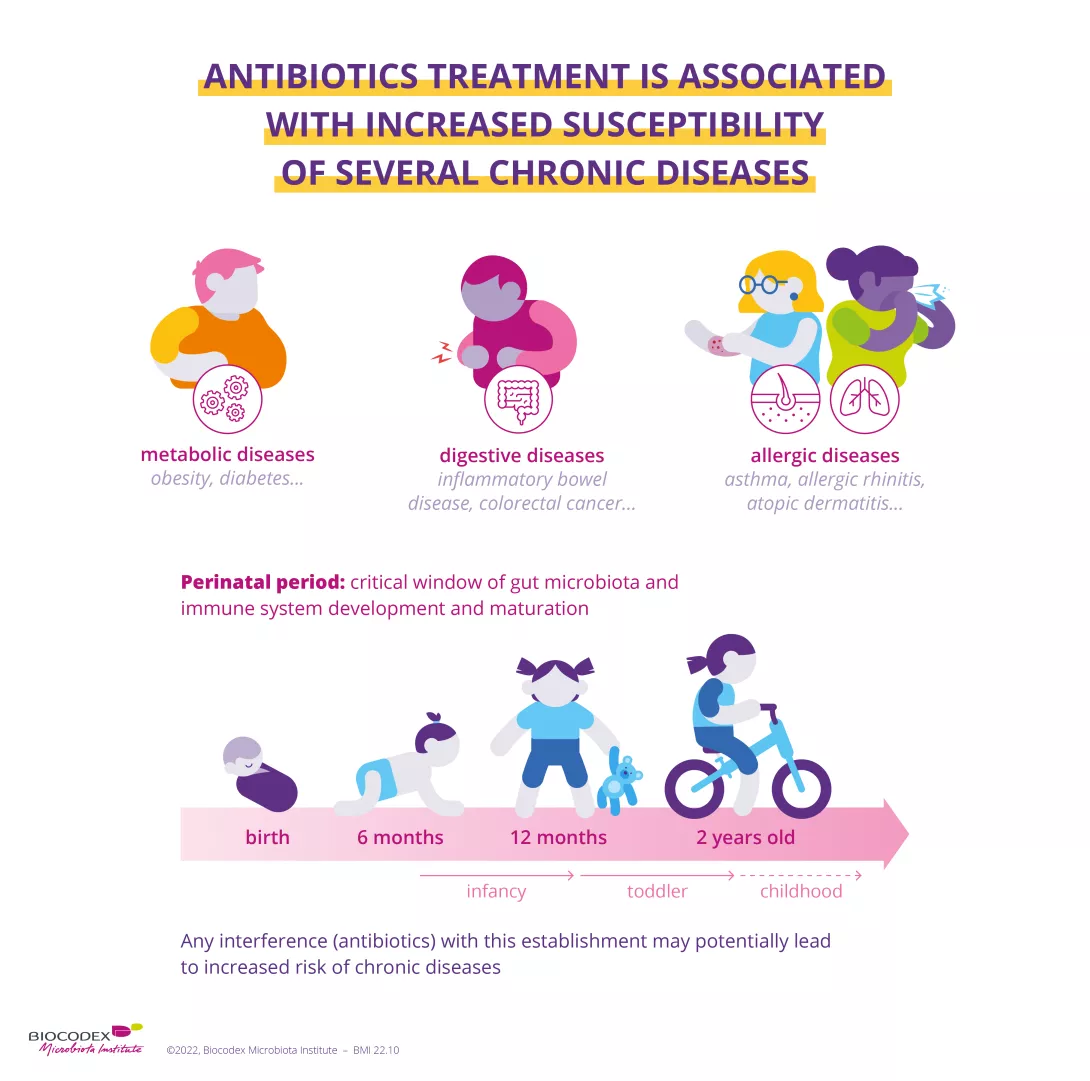
We are often told not to abuse antibiotics, but the use of antibiotics to treat conditions other than bacterial infections is still too common, with consequences for our health. Indeed, exposure to antibiotics during the first months of life may be associated with the subsequent development of asthma, an inflammatory disease of the (sidenote: https://www.who.int/news-room/q-a-detail/asthma ) . Alterations in the intestinal and nasal microbiota are recognized as a risk factor for the development of the disease and an indicator of its severity. Knowing that antibiotics alter bacterial communities, a team of researchers considered whether alterations of the nasal microbiota can explain the development of childhood asthma.
Antibiotics save life! Did you know that they also have an impact on your microbiota? Did you know that the misuse and overuse of antibiotics can lead to antibiotic resistance? Have you heard about the World AMR Awareness Week (WAAW)? All the answers in this dedicated page:
Antibiotics: what impact on the microbiota and on our health?
Link between antibiotics and asthma established
A team studied a group of around 700 children to search for a link between antibiotic exposure before the age of one and the development of asthma at the age of seven. In total, half of the children had received antibiotics in their first eleven months and almost 8% of them subsequently developed asthma. This proportion rose to over 11% among those treated with two or more antibiotics before eleven months, an increase of 4% compared to the children not exposed to antibiotics.
Moraxella, the main absentee from the nose
The researchers observed that the nasal microbiota changes during the first two years of life and that antibiotic therapy before the age of one impacts babies’ nasal flora, with this impact growing as the number of treatments increases. In particular, the absence from the nose of Moraxella–a bacterium often associated with respiratory diseases–seemed to signal an early and significant exposure to antibiotics. Their use before the age of one may therefore have long-term harmful effects on the nasal microbiota, facilitating the cascade of events that lead to the development of asthma. Even if other factors, such as the intestinal microbiota or the immune system, are also involved, these results still support current recommendations for the prudent use of antibiotics, especially among infants.
What is the World AMR Awareness Week?
Each year, since 2015, the WHO organizes the World AMR Awareness Week (WAAW), which aims to increase awareness of global antimicrobial resistance.
Antimicrobial resistance occurs when bacteria, viruses, parasites and fungi change over time and no longer respond to medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat, increasing the risk of disease spread, severe illness and death.
Held on 18-24 November, this campaign encourages the general public, healthcare professionals and decision-makers to use antibiotics, antivirals, antifungals and antiparasitics carefully, to prevent the further emergence of antimicrobial resistance.












