Antibiotics and neurodevelopmental disorders: does the microbiota play a role?
Antibiotics are often essential to treating certain infections from an early age. But by creating microbiota imbalances, might they influence the development of a child’s nervous system and contribute to disorders such as autism? A recent experimental study1 on mice provides the first – tentative – elements of an answer.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information

About this article
Neurodevelopmental disorders (NDD) such as autism or attention deficit hyperactivity disorder (ADHD) may be caused by disturbances in the first months of life when the central nervous system (brain, nerves, spinal cord, etc.) is under development. Their origin is still poorly understood, but many genetic and environmental factors are thought to be involved. Might antibiotics be among them?
Antibiotics
They have saved millions of lives but their excessive and inappropriate use has now raised serious concerns for health, notably with antibiotic resistance and microbiota dysbiosis. ach year, the WHO organizes the World Antimicrobial Awareness Week (WAAW) to increase awareness of antimicrobial resistance. Let’s take a look at this dedicated page:
Antibiotics: what impact on the microbiota and on our health?
Gut-brain axis suspected
According to a team of scientists in the US, a number of indications suggest this may be the case. The incidence of NDD has been rising sharply over the last few decades, with exposure to antibiotics only widespread since 1945. In the US, an average child receives nearly 3 courses of antibiotics before the age of 2, a critical period for neurodevelopment.
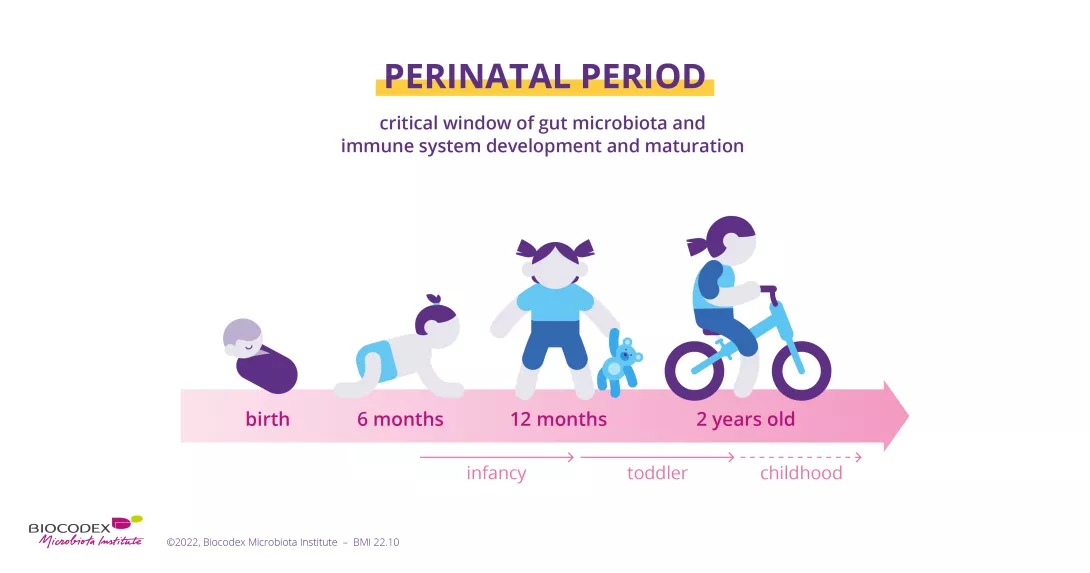
We also know that the gut acts as our “second brain” thanks to a biochemical “axis” of communication between the two organs. Recent research suggests that antibiotics taken during childhood disrupt the developing gut microbiota.2 At the same time, a link has been found between dysbiosis and various diseases, including neurological and psychiatric disorders.2
The researchers therefore administered very low doses of penicillin to newborn mice for three weeks. By comparing their microbiota to that of untreated mice, they found an alteration in their gut flora, notably a decrease in “good” bacteria, lactobacilli. Furthermore, they identified different activity between the two groups in 74 frontal cortex genes and 23 amygdala genes. These two parts of the brain are highly involved in emotional and cognitive functions and are also vulnerable to early disturbances. The researchers were also able to discover a link between certain microorganisms in the microbiota and genetic expressions in these brain areas.
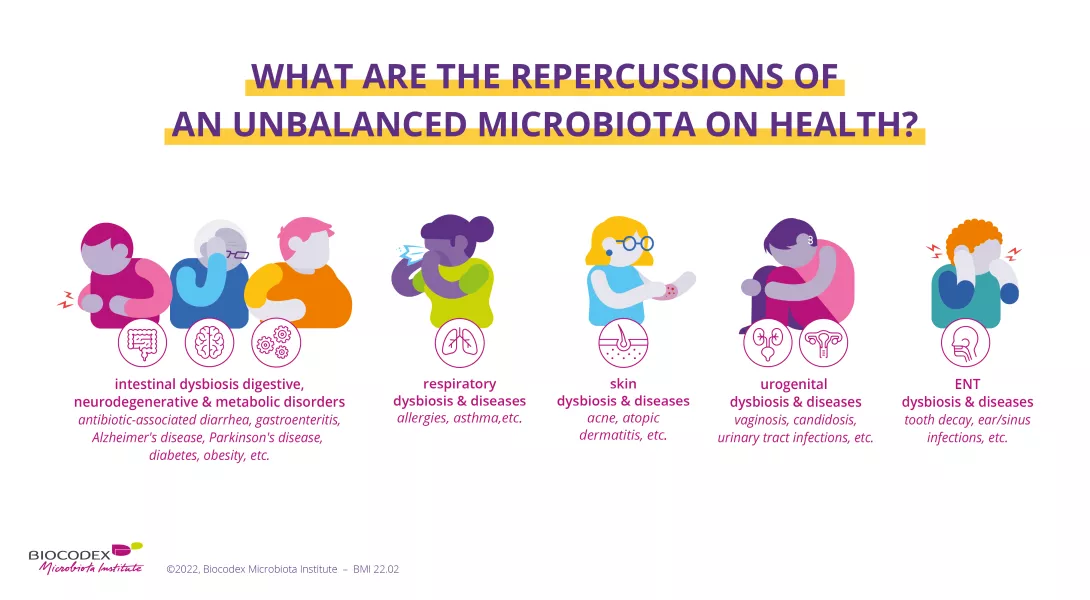
Role and impact of antibiotics on childhood neurodevelopment not yet explored
Therefore, in mice, antibiotics taken very early in life may, even at low doses, affect the activity of certain genes in brain areas (frontal cortex and amygdala) that are involved in NDD in humans. But the scientists remain cautious: they have not determined with certainty whether these changes in gene expression are directly caused by the antibiotics or by their effects on the microbiota. It also remains to be shown that these changes are significant for neurodevelopment. Moreover, results obtained in mice are not necessarily translatable to humans. They rather open new paths of research.
What is the World Antimicrobial Awareness Week?
Each year, since 2015, the WHO organizes the World Antimicrobial Awareness Week (WAAW), which aims to increase awareness of global antimicrobial resistance.
Antimicrobial resistance occurs when bacteria, viruses, parasites and fungi change over time and no longer respond to medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat, increasing the risk of disease spread, severe illness and death.
Held on 18-24 November, this campaign encourages the general public, healthcare professionals and decision-makers to use antibiotics, antivirals, antifungals and antiparasitics carefully, to prevent the further emergence of antimicrobial resistance.













