Skin diseases associated with a dysbiosis
The skin microbiota is a dynamic system in which microorganisms constantly compete to survive. Sometimes this balance breaks down, commensal bacteria become opportunistic pathogens1,4 and a dysbiosis results: it is a common feature in skin diseases (acne, psoriasis, dermatitis, etc.) and other non-pathological skin conditions (irritation, wounds, odors). However, it is not yet known whether dysbiosis is a cause or effect.2
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
About this article
Acne, psoriasis, rosacea... Many skin diseases are associated with a dysbiosis. This may have diagnostic or predictive value or even open up novel therapeutic approaches.
Skin cancer
Pathophysiology:
in many cutaneous neoplasms, dysbiosis appears to be involved in carcinogenesis.9,10,11,12 Conversely, a healthy microbiota may inhibit the development of tumors by regulating the immune system and controlling inflammation.
Role of the microbiota:
- S. aureus, Streptococcus pyogenes, Pseudomonas aeruginosa, the β-human papillomavirus, the Epstein Barr virus and Malassezia or Candida fungi may induce a state of chronic inflammation, leading to cancer;16
- link between S. aureus infection and severity of cutaneous T cell lymphoma.12
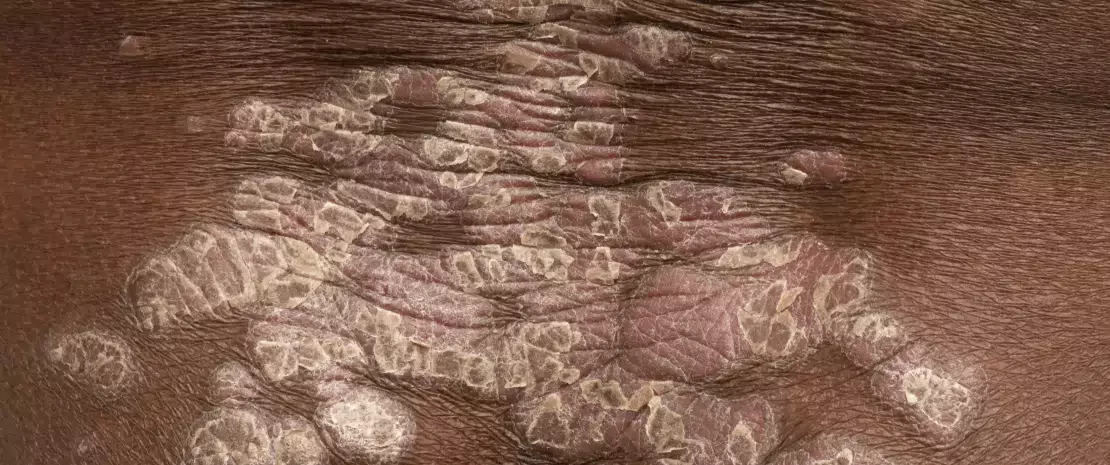
Psoriasis
Pathophysiology:
multifactorial immune-mediated disease, involving genetic factors, immune system disturbances and environmental triggers.13
Prevalence:
affects 2%-3% of the population, often appearing between 15 and 20 years of age11 with two common peaks of incidence (20-30 years of age and 50-60 years of age).13.
Role of the microbiota:
- psoriasis patients see an alteration in the composition of their skin microbiota and a loss of microbial diversity11, which affects not only the lesions, but the skin microbiota as a whole.11
- microorganisms associated with the disease still not clearly identified1,11, with numerous contradictory data. However, S. aureus thought to be more abundant and to participate in inflammation (by increasing the response of Th17 cells, which release pro-inflammatory cytokines);11
- often associated with gut dysbiosis.14
Acne
Pathophysiology:
multifactorial chronic inflammatory disease involving hyperseborrhea, abnormal keratinization of follicular ducts and a dysbiosis of the skin microbiota associated with a predominance of virulent C. acnes phylotypes.9
Prevalence:
8th most common skin disease, affecting 9.38% of the world’s population (all ages), with higher prevalence in adolescents, reaching 35%-100% in some countries.10
Role of the microbiota:
- loss of balance between the different C. acnes phylotypes (the more virulent phylotype IA1 becomes do minant and induces inflammation by activating the innate immune system);9
- loss of reciprocal control between C. acnes (maintains acidic pH, inhibits the development of S. epidermidis) and S. epidermidis (anti-inflammatory activity, limits the proliferation of C. acnes);9
- suspected secondary pro-inflammatory role (folliculitis) of opportunistic fungal species of the pilosebaceous apparatus (Malassezia and possibly Candida);11
- additional effect of diet on acne severity (interaction with gut microbiota).9
Atopic dermatitis (eczema)
Pathophysiology:
chronic inflammatory skin disease with a strong genetic component involving a disruption of the skin barrier and immune system (inflammatory Th2 cells), resulting in increased susceptibility to infections and allergens.11,15
Prevalence:
up to 20% of infants and 3% of adults worldwide11, and up to 10% of adults in developed countries.14
Role of the microbiota:
- patients see a loss of diversity in the skin microbiota11,12, both in lesions and healthy areas;
- increase in content of staphylococci, with a proliferation of S. aureus linked to a lower production of antimicrobial peptides by keratinocytes via the influence of Th2 cells.15 Increased presence of S. epidermidis in less severe forms;12
- a higher density of colonization with S. aureus correlated with more inflammation and increased disease severity.11
Seborrheic Dermatitis (SD) and Dandruff
Pathophysiology:
chronic skin disease involving a complex interaction between the Malassezia fungus, keratinocytes, and the inflammatory response induced by an altered lipid composition in the skin.12,18
Prevalence:
three peaks of incidence (early childhood, adolescence and from the age of 50 onwards). Half of adult population thought to be affected by DS and dandruff.11,18
Role of the microbiota:
- hydrolysis by Malassezia of skin lipids into free fatty acids that trigger an inflammatory response;16
- increased presence of Malassezia species, with M. restricta,M. globose and M. furfur the most commonly associated with seborrheic dermatitis. The first two species are the most virulent (they produce irritating oleic acids, leading to IL-8 and IL-17 activation);17
- Actinetobacter, Staphylococcus and Streptococcus dominate microbiota in the lesions;11
- correlation between disease severity and decreased bacterial diversity; no correlation with Malassezia abundance.12
Rosacea
Pathophysiology:
chronic inflammatory disease whose pathophysiology is not fully understood. Factors include neurovascular reactivity, genetic susceptibility, dysfunction of the innate immune responses, and comorbid gastrointestinal conditions.17
Prevalence:
between 0.9% and 10% of the population in the US and Europe.11
Role of the microbiota:
- Demodex folliculorum (a sebaceous gland mite) stimulates the production of inflammatory peptides and cellular growth factors. This mite may also carry Bacillus oleronius, a pro-inflammatory bacterium;11
- a variant of S. epidermidis, more virulent than the commensal bacterium, also thought to be involved;11
- often associated with a gut dysbiosis.18






