Melanoma: fecal microbiota transplant to overcome resistance to anti–PD-1?
A recent study published in Science shows that modulating the gut microbiota helps advanced melanoma patients respond to anti-PD-1 immunotherapy which their tumors had previously resisted. How? Thanks to fecal microbiota transplantation (FMT).
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Anti-PD-1 has been one of the major therapeutic advances of the past decade. It provides long-term clinical benefits to patients with advanced melanoma. In preclinical models and cancer patients, the efficacy of this therapy correlates with the composition of the gut microbiota. The aim of this Phase II clinical trial was to investigate whether resistance to anti–PD-1 can be overcome by modulating the gut microbiota.
Fecal microbiota and anti-PD-1: a winning combination?
The purpose of this clinical trial was to evaluate the safety and efficacy of FMT in combination with an anti-PD-1 agent (pembrolizumab) in metastatic melanoma patients previously refractory to this therapy. Fifteen patients received an anti-PD-1 (administered every 3 weeks until change) and a single FMT from seven donors who had previously shown a complete (4 patients) or partial (3 patients) response to immunotherapy. Radiographic assessments were performed every 12 weeks.
The gut microbiota of recipients and donors was analyzed via shotgun sequencing. For each recipient, one pre-FMT sample (collected 7 to 21 days beforehand) and all post-FMT samples (collected weekly for 12 weeks, then every 3 weeks) were sequenced. Patients’ progress was followed for 12 months on average.
FMT alters the gut microbiota
This combination was very well tolerated and provided significant clinical benefit in 6 patients, with regression or stabilization of the tumor for more than a year. In these patients, the median survival was 14 months.
The composition of the gut microbiota of the 15 FMT patients changed following FMT, regardless of whether the patient responded to immunotherapy. The gut microbiota composition of the 6 responders became more similar to that of the donors than did that of the non-responders. Their gut microbiota became richer in species of Firmicutes (Lachnospiraceae and Ruminococcaceae) and Actinobacteria (Bifidobacteriaceae and Coriobacteriaceae) and depleted in Bacteroidetes species.
FMT and immunotherapy reshape immune response
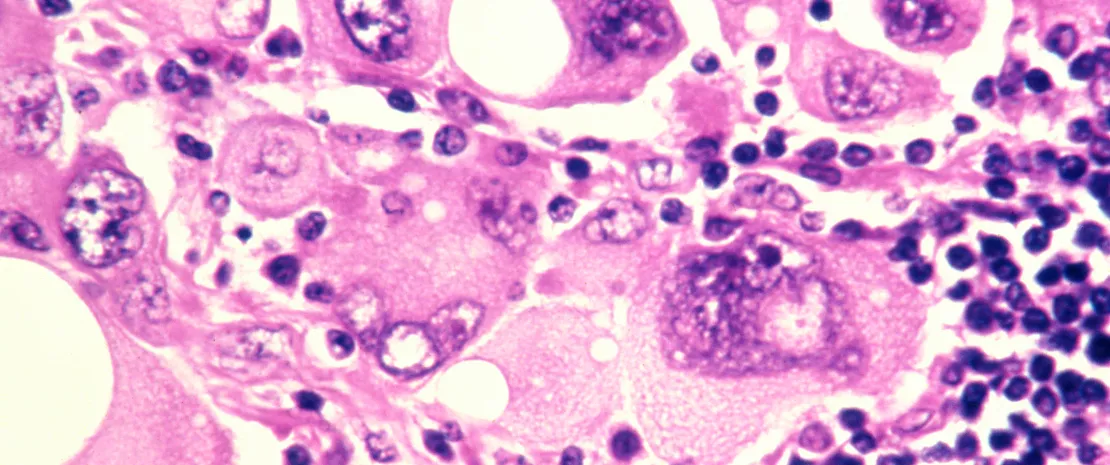
In the 6 responders, immunological changes in the blood and at tumor sites suggest increased activation of immune cells (increased CD8+ T cell activation, decreased frequency of IL-8). In addition, the responders had distinct proteomic and metabolomic signatures, with these changes apparently regulated by the gut microbiota. On the other hand, according to the researchers, non-responders may be refractory to immunotherapy for multiple reasons linked to the composition of their gut microbiota.
Although these findings require further investigation with broader clinical trials, the study suggests that a single FMT administered with a PD-1 inhibitor is enough to successfully change responders’ gut microbiota and reprogram the tumor microenvironment to overcome immunotherapy resistance. FMT changes the composition of the microbiota, improving the efficacy of anti-PD-1 therapy and inducing clinical responses in patients with immunotherapy-refractory melanoma.






