Your functional dyspepsia diagnosis check list
How many patients with persistent upper gastrointestinal discomfort do you see each week? How many remain undiagnosed with Functional Dyspepsia (FD)?
FD affects about 7% of adults3 but is often misdiagnosed due to overlapping symptoms with reflux, gastroparesis, and IBS. As a disorder of gut-brain interaction, it involves altered motility, microbiota imbalances, and psychological factors, making diagnosis challenging.
To help, Prof. Maura Corsetti, Prof. Nicholas Talley, and Prof. Lucas Wauters, in collaboration with the Biocodex Microbiota Institute, have developed a Functional Dyspepsia Diagnosis Checklist. This tool aids in more accurate diagnosis and clearer patient communication, improving management and care.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Authors
How to define functional dyspepsia?
Download your tool here
Functional dyspepsia (FD)
Often referred to as indigestion, is a common disorder of gut–brain interaction (DGBI) characterized by persistent upper abdominal symptoms with no evidence of structural disease.
Functional dyspepsia is a chronic and remitting disorder originating from the upper gastroduodenal region, characterized by one or more of the following symptoms2:

EPIGASTRIC PAIN
"It's like being stabbed from the inside out."

EPIGASTRIC BURNING
"My stomach burns like it's on fire."

EARLY SATIETY
(Inability to finish a meal)
"I feel full even if I don't eat much."

POSTPRANDIAL FULLNESS
(After a normal-sized meal)
"I feel like I have a stone in my stomach."
Functional dyspepsia is a highly prevalent DGBI based on strict Rome IV criteria:
7% of the global population is affected by Functional Dyspepsia
However, prevalence estimates vary depending on diagnostic criteria and geographic regions.
Functional dyspepsia is slightly more common in women than in men and can affect individuals of all ages. The condition is often underdiagnosed, as symptoms may overlap with other gastrointestinal disorders such as gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS). Despite its high prevalence, functional dyspepsia remains a challenging condition to manage due to its complex and multifactorial pathophysiology.
List of synonymous disorder names:
- Indigestion
- Gastritis,
- Non-ulcer dyspepsia
What to tell the patient ?
- The stomach and bowel talk to the brain, and the brain talks to the gut.
- A disorder of gut-brain interaction (DGBI)1 means the signalling is disturbed leading to symptoms. One common example of a DGBI is functional dyspepsia (FD).
- In Functional Dyspepsia the brain receives too many signals from the stomach which are normally filtered.
- Recurrent fullness (often called bloating), epigastric pain or burning and difficulty finishing a normal meal (early satiation), characterize this symptombased disorder named FD.
- Functional Dyspepsia is a disorder of gut-brain interaction, the two organs don’t communicate with each other properly.
- FD is a symptom-based disorder with no tissue damage.
- Gastrointestinal symptoms do not come alone, FD is often accompanied by higher levels of psychological upset such as anxiety, stress and depression.

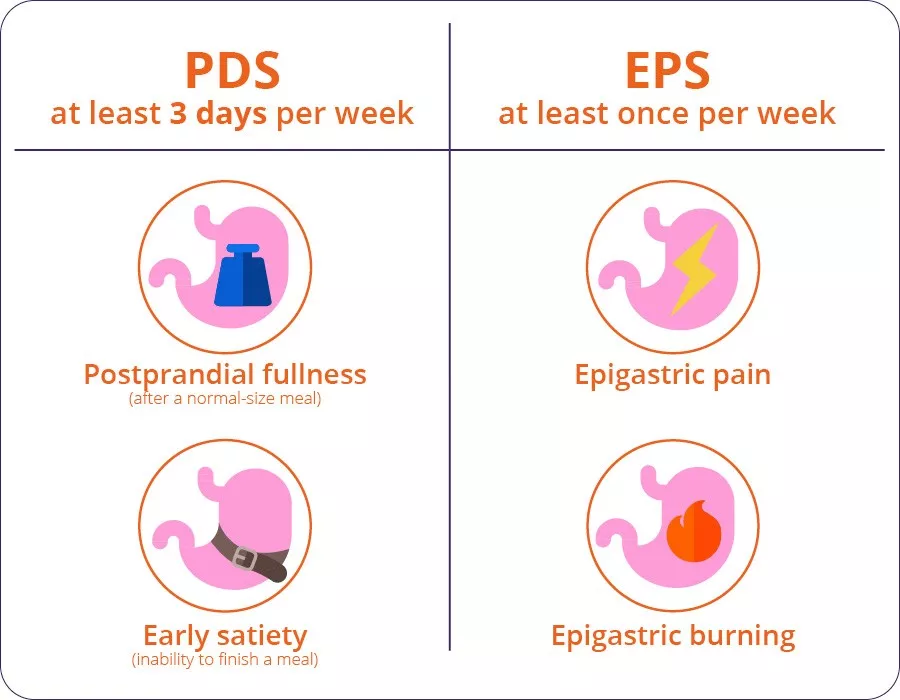
The two subtypes of Functional Dyspepsia
There are two subtypes of Functional Dyspepsia:
- EPS: Epigastric Pain Syndrome
- PDS: Postprandial Distress Syndrome which is the most common form
These two subtypes of dyspepsia sometimes overlap
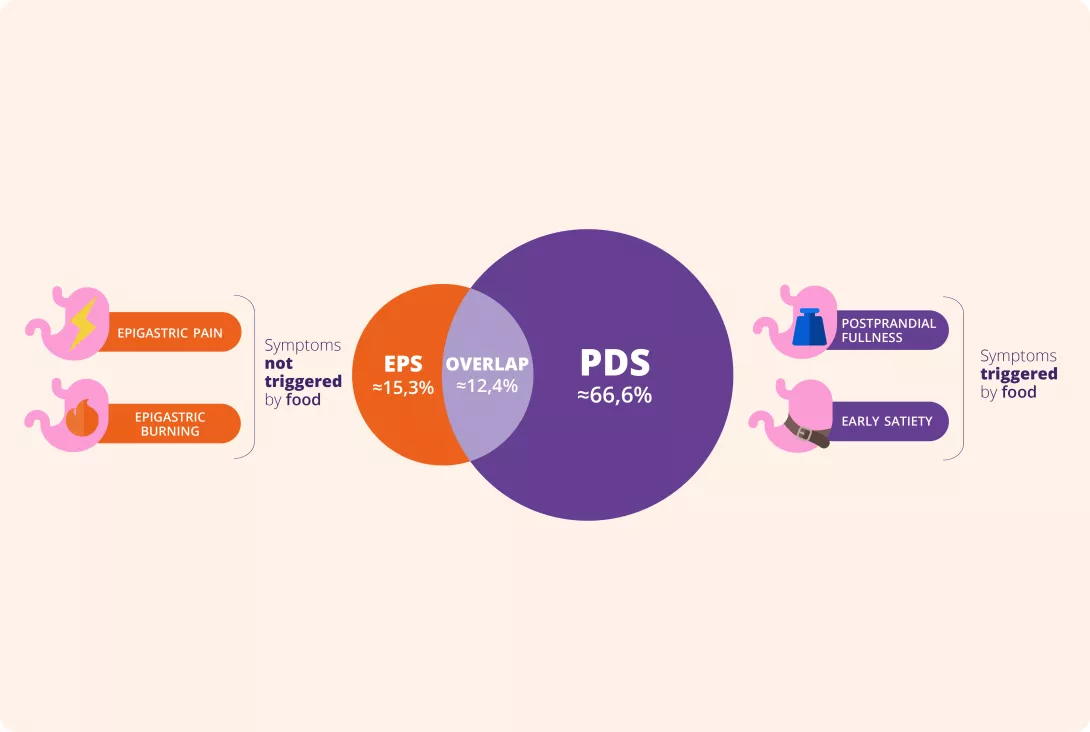
In the absence of a biomarker, diagnosis relies on symptom criteria of which the Rome IV criteria are the most recent and best validated. The Rome VI criteria classify patients into two functional dyspepsia subgroups:
- Postprandial distress syndrome (PDS), which is characterized by meal-induced symptoms,
- Epigastric pain syndrome (EPS), which refers to epigastric pain or epigastric burning that does not occur exclusively postprandially and can even be improved by meal ingestion

What do we know about the pathophysiology?
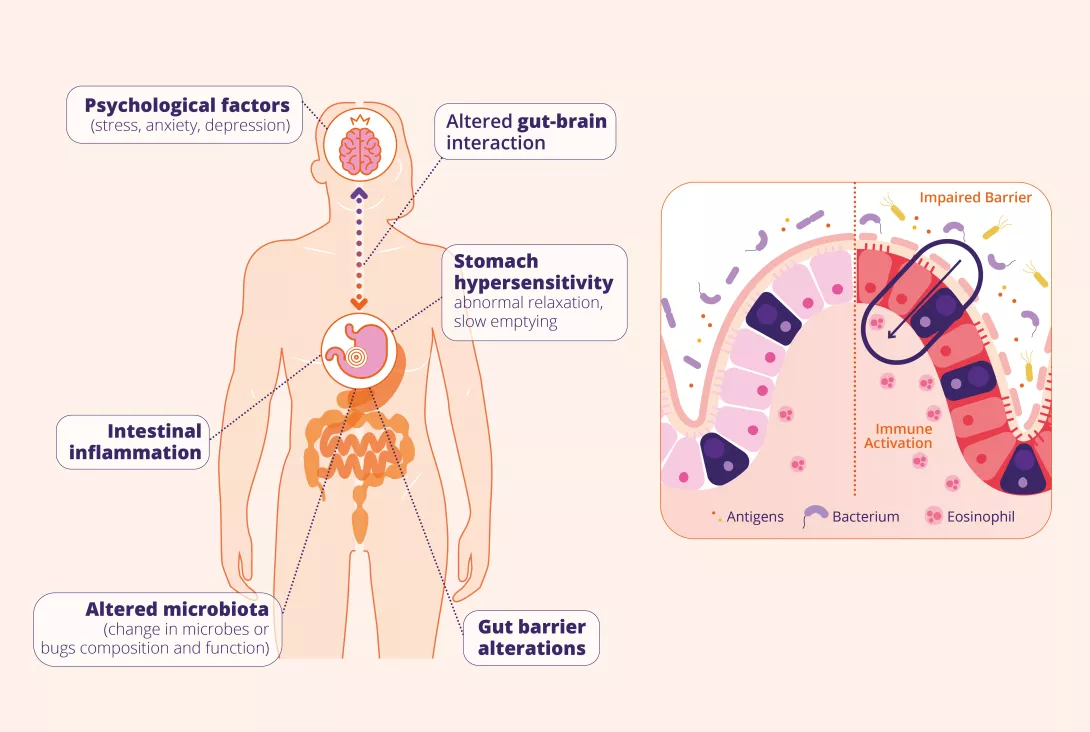
Although the precise pathophysiological mechanisms underlying functional dyspepsia are not yet fully understood and the precise etiology of the disorder remains elusive, recent evidence identified the following pathophysiological mechanisms1:
- Psycological factors: Altered gut-brain interaction: including stress and anxiety, influence gut function and may exacerbate symptoms
- Stomach hypersensitivity and dysmotility: Increased sensitivity of gastric and duodenal sensory neurons leads to exaggerated pain and discomfort in response to normal stimuli; disruptions in gastric motility, such as delayed gastric emptying, and impaired fundic accommodation
- Intestinal immune activation: Low-grade inflammation, particularly increased mast cells and eosinophils in the duodenum, contributes to symptoms
- Gut barrier alteration: A disrupted intestinal barrier allows food antigens and microbial products to penetrate the mucosa, potentially triggering immune activation
- Altered duodenal microbiota: Changes in the gut microbiota may contribute to immune activation, visceral hypersensitivity, and altered motility
These mechanisms interact in a complex manner, making functional dyspepsia a multifaceted disorder requiring a personalized approach to treatment.
What to tell the patient ?
- The microbial communities that live inside the gut are called microbiota.
- An unbalanced duodenal microbiota or dysbiosis, is a change in the composition and functions of the microorganisms that live in the gut.
- Food, bacteria, or substances found in the gut can sometimes cause the gut to malfunction and trigger symptoms.
- Functional Dyspepsia is a chronic disorder where symptoms can be managed through lifestyle changes, dietary therapy, medications and psychological therapies.
- We will meet every 2-3 months to follow up the effectiveness of the treatment/strategy.
How to make a confident diagnosis?
The diagnosis is based on symptoms according to Rome criteria2:
Question to ask: When do the symptoms start?
- Presence of at least one symptom severe enough to impact usual activities in the last past 3 months and at least for 6 months prior to diagnosis.
- and no evidence of structural disease (including on upper endoscopy) that is likely to explain the symptoms.
Risk factors
- Helicobacter pylori infection
- Being female
- Using certain pain relievers: such as aspirin and ibuprofen
- Smoking
- Anxiety or depression
- History of childhood physical or sexual abuse3
What are the warning signs to be excluded?
Check list of red flags to be investigated to confirm the diagnosis
- Age > 55 years* with new-onset dyspepsia
- Evidence of overt gastrointestinal bleeding including melena or haematemesis
- Dysphagia, especially if progressive, or odynophagia
- Persistent vomiting
- Unintentional weight loss
- Family history of gastric or oesophageal cancer
- Palpable abdominal or epigastric mass or abnormal adenopathy
- Evidence of iron-deficiency anaemia after blood testing5
*In regions with a high background prevalence rate of gastric cancer, such as Southeast Asia, a lower age threshold should be considered.
Refer to gastroenterologist for review

What investigations are needed ?
Recommended as routine tests:
- H. pylori test is recommended as the first one to be carried out: stool antigen, urea breath test
- Evaluation of the lower GI symptoms as IBS frequently overlaps with FD; essential to assess for celiac disease
- Assessment of the drug history (particularly about opioids, cannabis and NSAIDs)
Consider in specific case:
- Endoscopy for patients with recent onset symptoms and weight loss, and more than 55 years old; biopsy should be done if H. pylori status is unknown at endoscopy
- Gastric emptying (preferable scintigraphy) in case of nausea/ vomiting
Not useful as routine test:
- Blood testing
General management
The management of functional dyspepsia follows a multifaceted approach aimed at symptom relief and improving quality of life3,6,7

What are the general management concepts?
Lifestyle modifications, including:
- Dietary adjustments for limiting the intakes of potential dietary triggers (caffeine, spicy food…)
- A regular physical activity
- Good sleep habits
- And, probiotics intake
could help in reducing the symptoms.
A drug-based approach is privileged with acids suppressors (proton pump inhibitors, PPIs commonly used) and prokinetics.
Neuromodulators, such as tricyclic antidepressants, are used to modulate visceral hypersensitivity, alter pain perception, and improve symptoms in refractory cases
Cognitive behavior therapy, hypnotherapy, stress management, could play a key role in long-term symptom control
What to tell the patient ?
Most frenquently asked questions on Functional Dyspepsia:
Functional Dyspepsia can be treated but not cured. Recovery by itself is possible.
Functional Dyspepsia is not putting the patient at risk in developing any cancers.
FD is multifactorial disorder caused by altered gut sensitivity, motility, microbiota and communication between the gut and the brain.
Diet is relevant and constitutes a strong ally
Water does not improve Functional Dyspepsia.
Functional Dyspepsia does not increase the risk of death.
When to schedule follow-up care?
Follow-up approach depends on response to treatment (many non-responders)
2-3 months is a good interval for follow-up, with increasing intervals in case of treatment response Depending on the patient’s initiative