The gut microbiota and sleep disorder: a therapeutic approach based on modulation of the microbiota?
Research shows that the gut microbiota affects sleep by regulating the production of butyrate, a metabolite that effects neuronal activity in the hypothalamus. Could this open the way to treatments based on microbial balance?
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
The saying “Eat well, sleep well” is not wrong in implying a link between the digestive system and the brain: there does seem to exist a two-way relationship between sleep and the microbiota, involving the gut-brain axis. By which mechanisms does the gut microbiota affect sleep? This is the question that a team of researchers 1 tried to answer.
Roles of the microbiota and butyrate in mice
First step: the researchers studied the sleep of mice endowed with a gut microbiota without pathogens, and mice with no microbiota.
Result: the absence of the gut microbiota changed the structure of the sleep-wake cycle during phases of light and darkness. Reciprocally, the authors had previously shown that sleep deprivation went hand in hand with a reduction in butyrate levels (fecal and hypothalamic) in mice with a microbiota without pathogens, but not in mice with no microbiota.
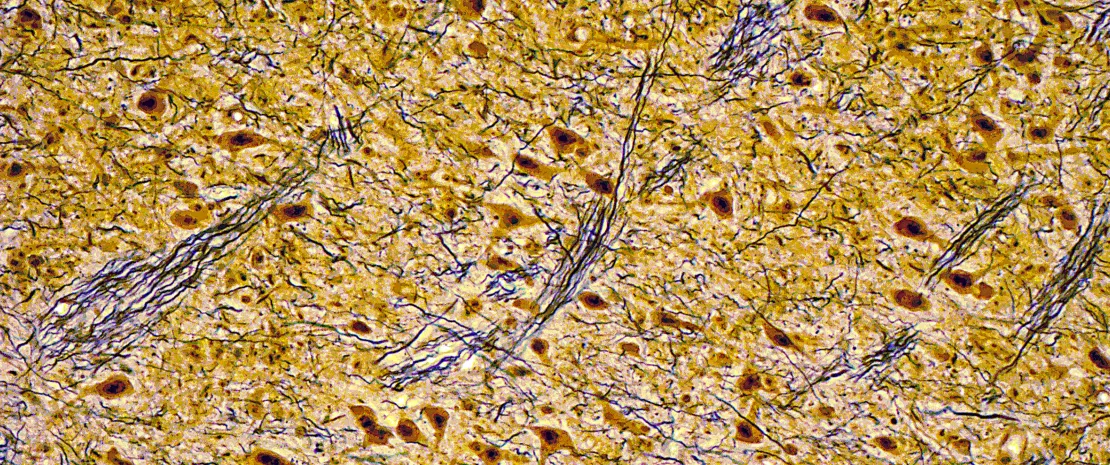
Next step: the researchers showed that the butyrate produced by gut bacteria could modulate neuronal function and promote sleep among the rodents. How? By inhibiting the neuronal activity of (sidenote: Orexin Neurotransmitters that regulate a wide variety of biological functions, most notably the sleep-wake cycle, reward and stress processing, alertness, vigilance, and cognitive functioning. Alterations of central and peripheral orexin levels are linked to conditions such as narcolepsy, anorexia nervosa, age-related cognitive decline, and neurodegenerative disease. Explore Toor B, Ray LB, Pozzobon A et al. Sleep, Orexin and Cognition. Front Neurol Neu… ) in the lateral hypothalamic region in mice.
40% Insomnia is often a chronic condition, with a 40% persistence rate over a 5-year period. ²
10-20% Approximately 10% of the adult population suffers from an insomnia disorder and another 20% experiences occasional insomnia symptoms. ²
Insomnia Women, older adults, and people with socioeconomic hardship are more vulnerable to insomnia. ²
Results confirmed in humans
Because the absence of gut microbiota can influence sleep behavior via a metabolic pathway, it remained to be confirmed that patients with insomnia presented with gut dysbiosis and changes in the microbial metabolism of butyrate. This was done in a new stage of the study, via stool samples from patients with insomnia and healthy volunteers: a lower (sidenote: Alpha diversity Number of species coexisting in a given environment ) and a significant reduction in 39 bacteria that produce butyrate were observed in those with insomnia. This explained the lower serum levels of butyrate among those who sleep poorly.
Transplantation of gut flora—and of sleep
Finally, in an attempt to show a causal relationship, gut flora from a patient with insomnia was transplanted to mice without flora. This transplantation reduced their blood levels of butyrate, activated the neurons of the lateral hypothalamus, and made the rodents insomniacs in turn. Oral administration of sodium butyrate improved the sleep of these rodents.
The researchers’ work showed a causal role for the gut microbiota-brain axis in regulation of sleep. The involvement of microbial metabolic pathways in sleep quality allows us to consider potential therapeutic strategies—via probiotics or butyrate—for the treatment of problems such as insomnia.








