Insomnia in seniors: a link with the gut microbiota
While it is estimated that one in two seniors suffers from chronic insomnia, a recent study1 demonstrates a link between sleep, cognition, and the gut microbiota in elderly insomniac individuals.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Difficulty in falling asleep or in staying asleep, waking up early... insomnia affects one in two adults over 65 years of age. With serious consequences for health since this chronic disorder is often accompanied by cognitive decline and increased mortality. Although the mechanisms are still poorly understood, an explanation of the link between insomnia and cognitive decline could lie in the gut microbiota-brain axis. A team of researchers therefore studied the links between the gut microbiota and the cognitive performance of 72 chronic insomniacs (of which 56 were women) with an average age of 73.2 years. Two factors were assessed, which generally testify to an accelerated cognitive decline during aging: sleep quality (objective measurement by (sidenote: Actigraphy Objective method of measuring sleep based on a device similar to a watch, worn on the wrist or ankle, which detects movements of the body and therefore waking activity. This apparatus thus measures the time taken to fall asleep, any periods of wakefulness and their duration, etc. ) over 2 weeks and subjective measurement by self-questionnaire) and cognitive performance (15 variables measured including 2 finally retained as being more discriminating).
50% Insomnia affects around 50% of the adult population over 65 years of age.
Sleep quality associated with intestinal dysbiosis
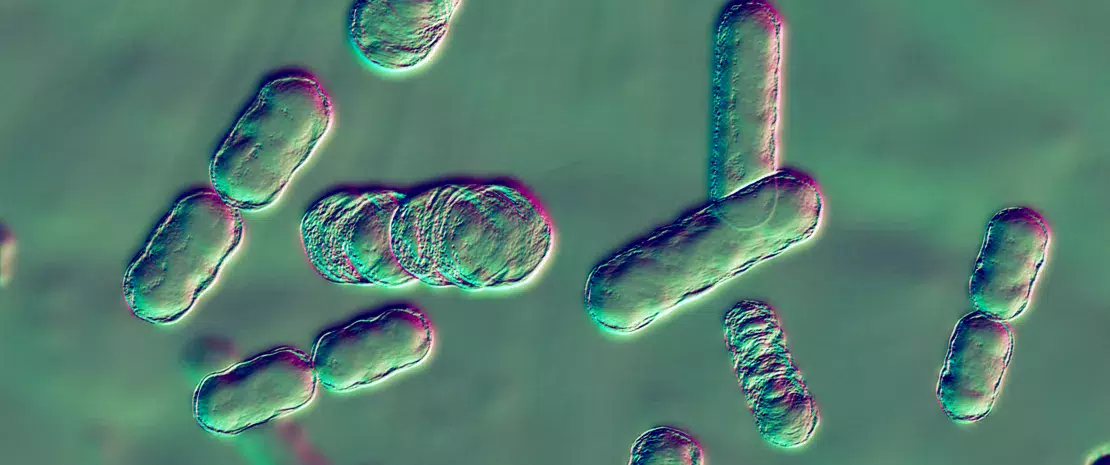
Analysis of stool samples of patients by sequencing of the 16S rRNA gene demonstrates the presence of 45 different phyla. Bacteroidetes were predominant (48%), followed by Firmicutes and, a long way behind, Proteobacteria (6 %), that is a decrease in Firmicutes and Proteobacteria in favor of the Bacteroidetes in comparison with patients without sleep problems2.
But above all, in the 72 insomniacs monitored, sleep efficacy (that is objective sleep not perceived sleep) and cognition explained 7.5 to 7.9% of the total variation in the composition of the gut microbiota (in terms of (sidenote: Amplicon Sequence Variant (ASV) Term designating individual DNA sequences recovered from a marker gene analysis (“parasite” sequences induced by gene amplification and sequencing are eliminated by this technique). This method is therefore distinguished from OTU counts, (Operational Taxonomic Unit), more commonly used, where bacteria are grouped together based on similarities of a given gene serving as a taxonomic marker. ) ). That is a significant impact, comparable to that caused by medicines, blood parameters, intestinal transit, diet, state of health, and anthropometric data, according to a previous study3.
Lachnoclostridium and Blautia involved?
In addition, the correlation analysis showed that a strong presence of the genus Lachnoclostridium went together with effective sleep and higher cognitive performance (shorter response time). Conversely, decreased cognitive performance was associated with greater abundance of the genus Blautia.
This study provides a new building block in the relationship between insomnia, cognition, and the gut microbiota. Although it does not allow any causality to be inferred, it points the finger at the gut microbiota as a potential aid to the diagnosis of elderly persons suffering from sleep disorders and cognitive decline, even as a new therapeutic target in the field of aging.
Recommended by our community

"True!" - DOKI DE LAGOS (From Biocodex Microbiota Institute on X)






