Antibiotics and risk of IBD in adults
According to a new study published in The Lancet Gastroenterology & Hepatology, high antibiotic exposure in adults may be associated with an increased risk of inflammatory bowel disease (IBD), regardless of genetic predisposition and childhood exposure factors.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
In recent years, the incidence of IBD has increased alarmingly worldwide. Risk factors thought to be involved in the development of IBD include genetic predisposition, environmental factors (hygiene, antibiotics, etc.) and gut microbiota disorders. Antibiotic use in the first years of life has been linked to a risk of IBD in children, but data are scarcer and remain controversial for adults. In a large prospective case-control study, a team examined the relationship between antibiotic therapy and the risk of IBD.
Swedish population scrutinized
To select their patients, the authors used the information generated by the (sidenote: ESPRESSO Epidemiology Strengthened by histoPathology Reports in Sweden ) study gathering all reports of gastrointestinal diseases in Sweden from 1965 to 2016 and cross-checked them with the Swedish Patient Register and Prescribed Drug Register. The authors then identified in the general population up to five control subjects per patient, matched by age, gender, place of residence and calendar year. Lastly, unaffected siblings were also included in the study as a secondary control group sharing genetic or environmental risk factors with the patients. In total, 23,982 patients with IBD aged 16 to 65, 117,827 control subjects and 28,732 siblings were included.
Hailed as one of the greatest medical advances of the 20th century, antibiotics have saved millions of lives. But they also have an impact on our microbiota by inducing a dysbiosis. Let’s take a look at this ambivalence role:
The ambivalent role of antibiotics
Twice the risk of developing IBD
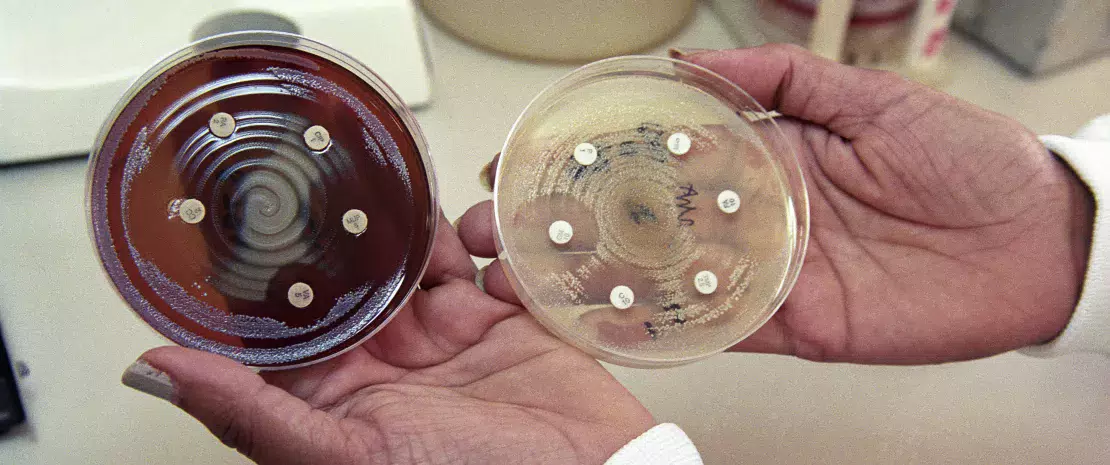
According to the study, antibiotic use was associated with a 1.88-times increase in the risk of developing IBD. For ulcerative colitis (UC) and Crohn’s disease the risk increased by 1.74 and 2.27 times, respectively. The risk also increased with the number of antibiotic prescriptions and when the antibiotics used had broad-spectrum activity. For the authors, this result supports the hypothesis that a gut microbiota dysbiosis caused by antibiotic treatment may lead to dysfunction of the intestinal barrier and local inflammatory response, resulting in an increased risk of developing IBD.
What is the World AMR Awareness Week?
Each year, since 2015, the WHO organizes the World AMR Awareness Week (WAAW), which aims to increase awareness of global antimicrobial resistance.
Held on 18-24 November, this campaign encourages the general public, healthcare professionals and decision-makers to use antimicrobials carefully, to prevent the further emergence of antimicrobial resistance.
Exposure to antibiotics: an independent risk?
Although tenuous, a link between antibiotic treatment and IBD risk was also observed among individuals who shared a genetic predisposition and exposure factors during childhood, i.e. when patients were compared to their siblings as a control population. Further research is required to investigate the mechanisms by which antibiotics modify the gut microbiota, leading to the development of IBD. Nevertheless, according to the authors, this is one more argument in favor of a cautious and targeted use of antibiotics.





