Urinary tract infections: toward alternative dietary and probiotic strategies?
Preventive strategies based on a balanced diet or even the use of probiotics could represent alternatives to curative treatment with antibiotics in the management of urinary tract infections. Although effective in the short term, antibiotics can also lead to dysbiosis, new infections and resistance.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
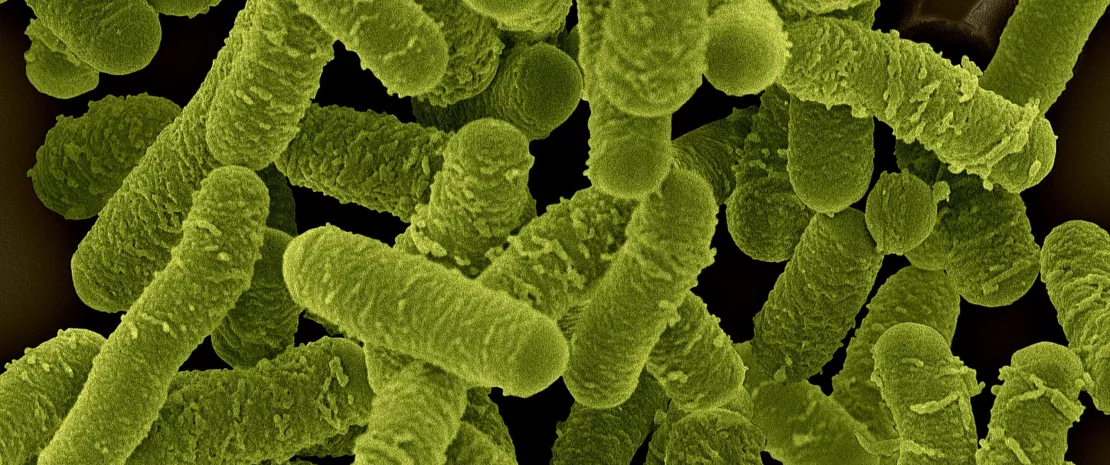
Over 80% of urinary tract infections are caused by (sidenote: Uropathogenic Escherichia coli E. coli that often have additional genes (compared with commensal E. coli) which boost their virulence (flagella, toxins, surface polysaccharides, etc.). ) . These gut bacteria can migrate from the anus, colonize the urethra and then migrate up into the bladder. In fact, previous studies have shown that women suffering from urinary tract infections have an increased abundance of E. coli in their digestive system, with similarities between the gut species and those colonizing the urinary tract.
To assess dysbiosis and other potential risk factors in women with a history of cystitis, researchers enrolled 753 female volunteers aged 18 to 45 who had been diagnosed with a UTI in the last five years and were otherwise in good health. 1
With the exception of a spike among young women aged 14-24, the prevalence of urinary tract infections increases with age. The prevalence in women over 65 years of age is approximately 20%, compared with approximately 11% in the overall population. 2
Between 50% and 60% of adult women will have at least one urinary tract infection in their lifetime, and close to 10% of postmenopausal women indicate that they had a urinary tract infection in the previous year. 2
Opt for a healthier diet
Nearly ¾ of the women studied (71%) had gut dysbiosis, which proved to be associated not only with the (sidenote: Recurrent urinary tract infection A recurrent urinary tract infection is defined as the occurrence of ⩾2 symptomatic episodes in 6 months or ⩾3 symptomatic episodes in 12 months. ) of their urinary tract infections, but also with the presence of antibiotic multidrug resistance in their flora.
Another particularity of the population studied is their diet, whether it be drinks (less than 1 L of water per day, consumption of sugary drinks), food (over-representation of salty products, high-calorie diets rich in added sugars and saturated fats), or dietary supplements intended to prevent urinary tract infections.
More than 80% of urinary tract infections are caused by uropathogenic Escherichia coli. ¹
150 million Urinary tract infections are among the most frequent bacterial diseases, affecting an astounding 150 million individuals worldwide each year. ¹
For the researchers, these observations support the link between diet and the composition of the gut microbiota. In this regard, they refer to previous studies which have shown that only 12% of structural variation in the gut microbiota can be attributed to genetic changes, while 57% can be explained by dietary changes.
Microbiota as a new therapeutic strategy
Although the standard treatment for urinary tract infections is antibiotics, in the long term they disrupt the gut microbiota (dysbiosis) and encourage multidrug resistant organisms. Hence the importance, according to the authors, of alternative and complementary therapeutic choices.
The researchers also point out the beneficial effects of probiotics, in particular Lactobacillus spp. which reduces the adherence, growth and colonization of uropathogenic bacteria such as E. coli: Enteric-release L. salivarius travels to and protects the urinary and vaginal microbiota, and a probiotic composed of two strains of Lactobacillus and cranberry extracts significantly reduces the number of recurrent urinary tract infections in young premenopausal women, compared with a placebo product.
Probiotics also have a major advantage over antibiotics: the administration of lactobacilli does not encourage the development of resistance.









