Idiopathic urethritis in men: new infectious etiologies?
Male idiopathic urethritis is treated largely using probabilistic antibiotic therapy. Researchers1 seeking a more targeted approach to these common infections have analyzed the urinary and urethral microbiota of symptomatic subjects, giving consideration also to their sexual orientation. They have identified “new” bacteria potentially involved in such infections, including Haemophilus influenzae.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
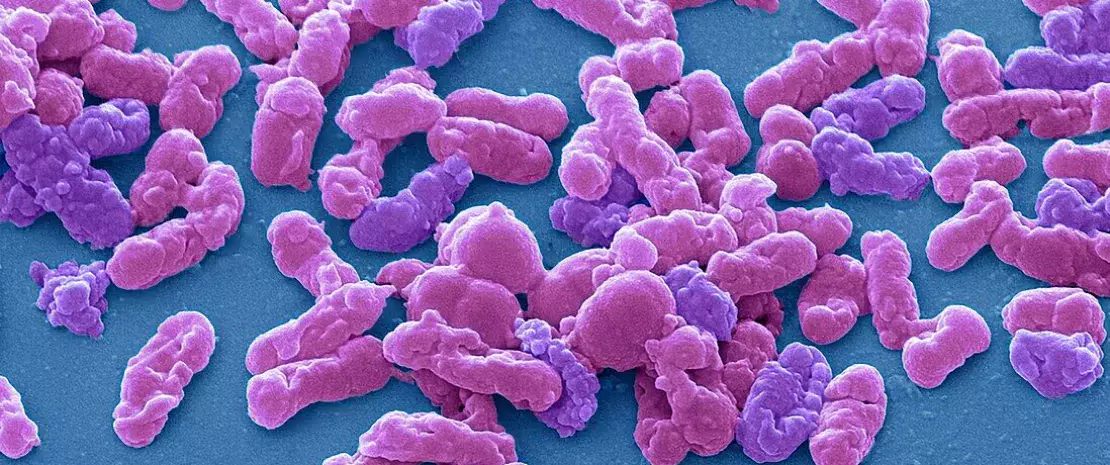
Urethritis is a sexually transmitted infection (STI) caused mainly by Neisseria gonorrhoeae, but also by Chlamydia trachomatis or Mycoplasma genitalium, and less commonly by a virus, such as herpes simplex. But up to 50% of non-gonococcal urethritis is considered to be idiopathic. In rare cases it is non-infectious and of undetermined etiology, which poses a diagnostic and therapeutic challenge for clinicians. Probabilistic antibiotic therapy is used widely in such cases, but can result in inadequate or excessive treatment with a risk of antibiotic resistance. Recent studies also suggest that the infectious agents responsible for non-gonococcal urethritis in men who have sex with women (MSW) are not the same as in those who have sex with men (MSM).
Exploration of urinary and urethral microbiota in relation to sexual orientation
Some Australian researchers sought to determine which infectious agents, apart from those already known, might contribute to non-gonococcal urethritis in men, taking into account their sexual practices and the biological sex of their partner. For this, they conducted a case study including 199 men, 96 of whom had symptoms of idiopathic urethritis and 103 of whom did not, who served as controls. The median age of participants was 31 years, 73 had had a sexual relationship with a man in the month prior to inclusion (classified as MSM), and the remainder were classified as MSW. For all of them, the researchers had samples of urinary and urethral microbiota available for sequencing analysis.
Urethritis not always “idiopathic”: hope for more targeted treatments
Their results revealed that Haemophilus influenzae, which naturally colonizes nasopharyngeal microbiota, was more abundant in MSM participants with idiopathic urethritis. In addition, H. influenzae was clearly associated with clinical features such as urethral burning, dysuria and purulent discharge. The researchers believe having oral sex without a condom could be the main mode of contamination by this bacterium. They observed more of the genus Corynebacterium in affected MSW, which they found surprising since it is considered commensal in male genital microbiota. The scientists conclude that some specific species of Corynebacterium may become pathogenic when present in abundance. There were also more Ureaplasma, Staphylococcus haemolyticus, Streptococcus pyogenes, Escherichia and Streptococcus pneumoniae in the urinary and urethral microbiota of symptomatic subjects, so they may all promote urethritis.
Possible infectious causes of non-gonococcal urethritis, previously described as idiopathic, have thus been discovered. If these results are confirmed by other studies, doctors may eventually be able to offer their patients more targeted treatments.








