Microbiota and Infection Diarrhea: virtuous or vicious circle ?
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections

About this article
INFECTIOUS DIARRHEA, ONE OF THE LEADING CAUSES OF INFANT MORTALITY WORLDWIDE
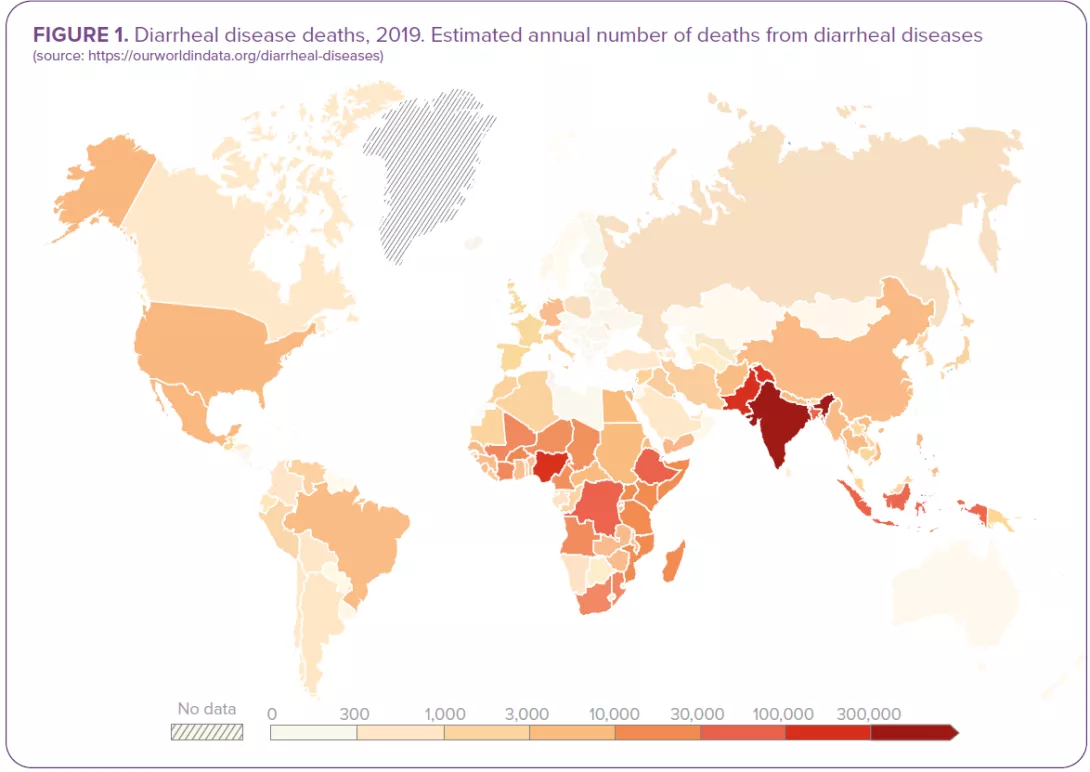
The passage of 3 or more loose or liquid stools per day corresponds to the common definition of diarrhea as set out by the WHO.1 Both criteria (frequency and consistency) are necessary: frequent passing of formed stools is not diarrhea, nor is the passing of loose stools by breastfed babies (Figure 1). 1.6 million deaths were attributed to diarrhea in 2016.2 Children are particularly at risk: diarrheal disease is the 3rd leading cause of death in children under 5 years of age. A large part of the mortality used to be attributed to severe dehydration linked to fluid loss but today, septic bacterial infections account for an increasing proportion of all diarrhea-associated deaths.1 Malnourished or immunity-impaired children are the most at risk of life-threatening diarrhea, as well as people living with HIV.1
DIARRHEA CLASSIFICATION
There are 3 clinical types of diarrhea based on its symptoms and duration:1
- acute watery diarrhea, which lasts several hours or days (up to 14 days) and includes cholera;
- acute bloody diarrhea (dysentery);
- persistent diarrhea, which lasts 14 days or longer.
Most cases of acute diarrhea are due to infections:1,3,4 a virus, bacteria or parasites could all be responsible, but rotavirus and Escherichia coli are the two most common etiological agents of moderate-to-severe diarrhea in low-income countries.1 Rotavirus and Shigella are responsible for the highest number of infectious-diarrhea related deaths;2 this is giving rise to preventive vaccination strategies (still under development for the latter). Although certain fungal communities have been confirmed to be associated with diarrhea, the role of fungi in diarrhea remains controversial.5 They could be at work in some clinical settings, especially in immunocompromised patients prone to invasive fungal infections (candidiasis).6
PATHOPHYSIOLOGICAL SYNDROMES OF DIARRHEA
From the clinical perspective, diarrheagenic pathogens can cause 2 pathophysiological syndromes:4
- Noninflammatory diarrhea (NID): patients present with nausea, vomiting, watery and voluminous stools, and abdominal cramping resulting from intestinal secretion (the intestinal mucosa remains intact). This milder course of disease is usually viral (Rotavirus, Norovirus…) but it can also be bacterial (enterotoxigenic Escherichia coli, Clostridium perfringens…) or parasitic (Giardia, …);
- Inflammatory diarrhea (ID): patients present with fever, abdominal pain, tenesmus and bloody stools of smaller volume than in NID. This severe course of disease is usually caused by invasive or toxinproducing bacterial strains (Shigella, Salmonella species…) that lead to mucosal barrier disruption and tissue destruction.
“Rotavirus and Escherichia coli are the two most common etiological agents of moderate-to-severe diarrhea in low-income countries.”
BEHIND THE SCENES OF DIARRHEA: THE MICROBIOTA
VICIOUS CIRCLE: WHEN DIARRHEA LEADS TO GUT DYSBIOSIS
Infectious diarrhea is regarded as a major dysbiotic event resulting from:
- increased bowel movements and disruption to mucosal integrity, 3
- increased proportion of water in the fecal matter and reduced transit time which contributes to taxonomic scarcity, 3
- and possible oral rehydration, zinc supplements, probiotics and even antimicrobials (in the case of dysentery or bacterial infections) which also contribute to an imbalance in the intestinal microbiota.7
Depending of the type of infection, infectious diarrheas are usually accompanied by dysbiotic states: 7 bacteria-induced diarrhea is generally linked to an elevation in Escherichia, Streptococcus and oral bacteria; viral infections lead to a less pronounced reduction in anaerobic commensals in the gut (higher abundance in Bifidobacterium); giardia-induced diarrhea is linked to a decrease in Gammaproteobacteria and an enrichment in Prevotella.
“The community of microbes that inhabit the gut is as numerous as human cells, with the vast majority of bacteria residing in the colon.” 8
Dysbiosis corresponds to the disruption of a formerly stable, functionally complete microbiota.9
The community of microorganisms - bacteria, viruses, fungi (including yeasts) and parasites - that inhabit the gut.10
VIRTUOUS CIRCLE: WHEN THE GUT MICROBIOTA OFFERS PROTECTION
Mechanisms by which the gut microbiota provides colonization resistance can be both direct and indirect. The microbiota directly inhibits diarrheal pathogens mainly via competition for nutrients, but also by limiting in a variety of ways the growth of diarrheal pathogens: secreting bacteriocins (antimicrobial peptides), cell contact-dependent inhibitory structures (type VI secretion system), producing molecules that reduce the pathogens’ virulence…
The microbiota also indirectly inhibits diarrheal pathogens via its effects on the host: by promoting gut barrier maintenance and by stimulating both the innate and the adaptive immune system.8
HOW TO MANAGE INFECTIOUS DIARRHEA?
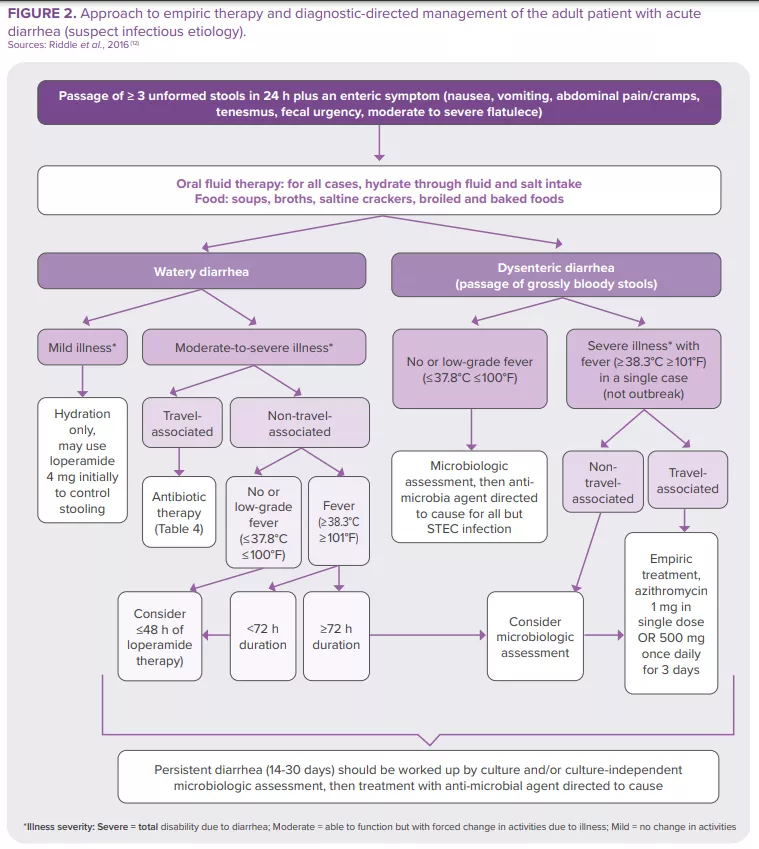
The majority of intestinal infections are self-limiting in immunocompetent individuals. Nevertheless, some patients (with severe dehydration, more severe illness, persistent fever, bloody stools, immunosuppression…) require specific diagnostic investigation. These can include a complete blood count, a creatinine and electrolytes assessment, verification of leukocytes and lactoferrin presence in the stools, stool culture, along with C. difficile testing, PCR, ova and parasites search, endoscopy and abdominal imaging11. The American College of Gastroenterology (ACG) guideline12 provides recommendations for the diagnosis and management of adult patients presenting with acute diarrhea of suspect infectious etiology (Figure 2). Clinical investigation in children is based on the same principles.23 In 2023, World Gastroenterology Organisation Global Guidelines included probiotics in the prevention and treatment of some infectious diarrhea57.
World Gastroenterology Organisation Global Guidelines, 2023
Treatment of acute diarrhea: “oral administration [of some probiotic strains] shortens the duration of acute diarrheal illness in children by approximately 1 day.”57
Prevention of:
- acute diarrhea: “probiotics probably make little or no difference with diarrhea lasting 48 hours or longer.”
- antibiotic-associated diarrhea: “probiotics may provide a moderate effect for preventing antibiotic-associated diarrhea in children, adults, and elderly adults.”
- Clostridioides difficile diarrhea: “probiotics are effective for preventing C. difficile–associated diarrhea in patients receiving antibiotics.”



