Antibiotics disrupt cancer immunotherapy via gut and immune effects
Prior antibiotics administration is shown to reduce efficacy of Immune checkpoint inhibitors and alter microbiome makeup and immune response in advanced gastric cancer.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Author
Mounting evidence reveals that the gut microbiome influences how well immune checkpoint inhibitors (ICIs) like PD-1 inhibitors work against cancer. But whether antibiotics given shortly before immunotherapy impact outcomes remained unclear, especially in advanced gastric cancer—until now.
In a groundbreaking study published in Cell Reports Medicine 1, an international research team provides compelling data from 329 patients that taking antibiotics within one month of starting PD-1 blockade unleashes negative consequences.
Ranked as the fifth most prevalent cancer worldwide, advanced gastric cancer stands as the third leading cause of global cancer-related mortality. 2
Analytics illuminate survival gap
The multi-center analysis discovered that 44-46% of advanced gastric cancer patients had taken antibiotics within 28 days pre-immunotherapy. This prior antibiotic (pATB) group experienced markedly lower response rates (1.5% vs 11.8%) and shorter survival time compared to the non-pATB group when given (sidenote: Anti-PD-1 immunotherapy based on immune checkpoint inhibitors that target the PD-1 checkpoint, reversing the deactivation by the tumor of the recognition system associated with the PD-1 protein present on the surface of T lymphocytes. The immune system’s effectiveness against tumor cells is thus restored. ) medications (pembrolizumab or nivolumab).
Strikingly, no survival difference occurred with pre-chemo antibiotics group (N=101 patients that received irinotecan as chemotherapy), pointing to an immunotherapy-specific mechanisms.
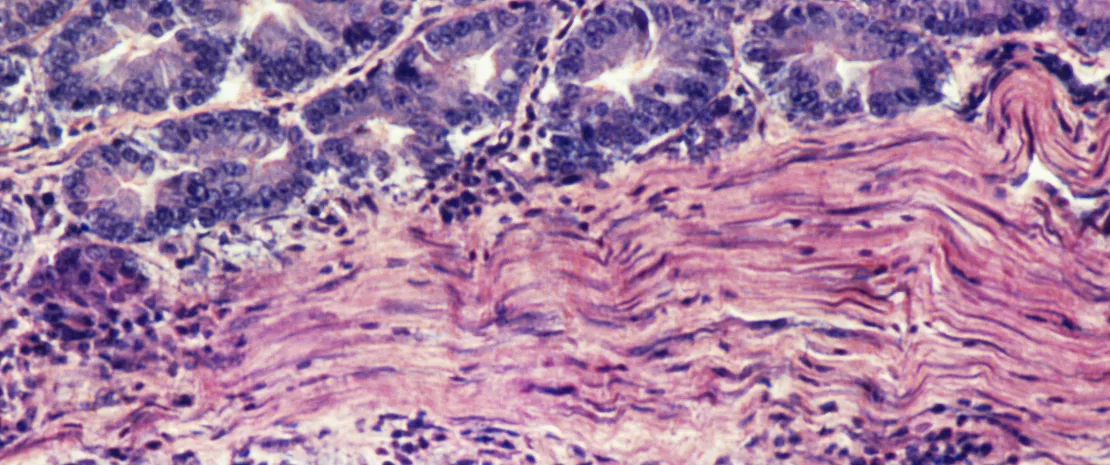
Microbiome and immune system disruption
To unravel these mechanisms, the team performed microbiome gene sequencing on bacterial genomic DNA extracted from stool samples from 24 PD-1-treated patients. This quantified bacteria species and abundance changes due to antibiotics.
Additionally, they sequenced blood immune cells at the single cell level, enabling intricate comparison of cell subset frequencies and properties.
The researchers uncovered two major interconnected effects of pATB exposure that can foil PD-1 inhibitor efficacy:
- Reduced overall diversity of intestinal bacteria, including fewer “good bacteria” like Lactobacillus gasseri.
- Rise in exhausted CD8+ T cells overloaded with PD-1 and other inhibitory immune checkpoints rather than more robust effector T cells.
Further computational analyses demonstrated that the microbiome and immune metrics statistically associated with patient outcomes: For example, higher Lactobacillus gasseri abundance was linked to longer progression-free and overall survival. Conversely, disproportional enrichment of circulating exhaustiveCD8+ T cell frequency predicted worse prognosis.
Caution urged when prescribing antibiotics
The authors strongly advise clinicians to carefully weigh the antibiotic necessity and seek alternatives before immunotherapy initiation. ATBs should be prescribed with caution in patients with AGC who are planning to receive PD-1 inhibitors. They suggest prospectively validating microbiome-modulating interventions like fecal transplants to rescue pATB patients’ treatment response.
This study revealed a critical piece of the cancer immunotherapy puzzle highlighting the microbiome's role. Further large prospective studies accompanied by translational analysis would confirm the findings of this study, this discovery opens promising doors for boosting clinical outcomes in advanced stomach cancer and beyond.









