In adults
The FGIDs encountered in adults are functional diarrhea, functional bloating, and especially IBS and functional constipation. As in children, their etiology is poorly understood.13,14,15
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
About this article
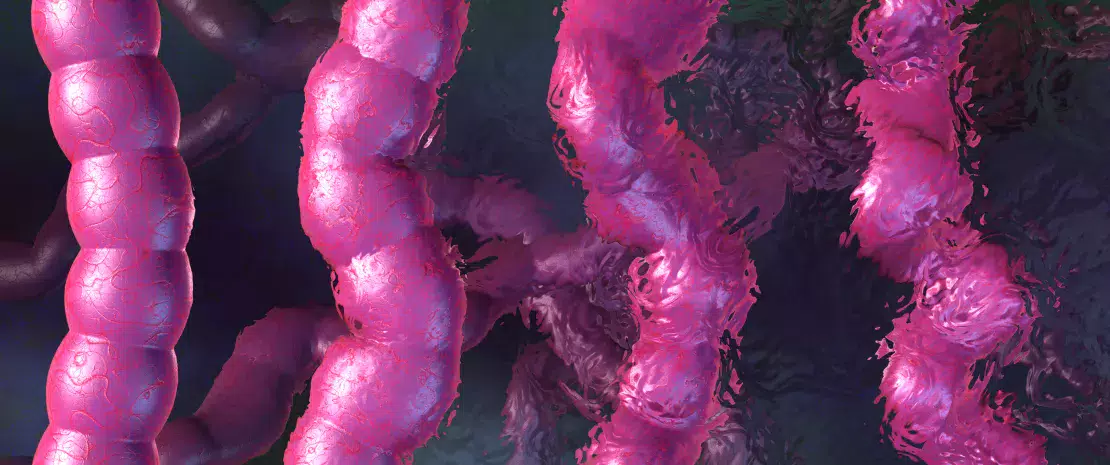
A MICROBIAL SIGNATURE
An Italian team has suggested the hypothesis that bacterial and biological markers (SCFA) could be used to discriminate between the different subtypes of IBS, a disorder that affects between 7% to 21% of the general population depending on the countries under consideration. Characterization of the fecal samples of 40 patients suffering from IBS (5 samples collected at 4 week intervals) demonstrated that certain bacterial species enabled the different IBS subtypes to be discriminated: in particular, greater abundance of bacteria belonging to the Ruminococcaceae and Lachnospiraceae families were observed in the IBS C subtype compared to the IBS-D subtype. Fecal concentrations of SCFA would also seem to be effective markers for discrimination of the different subtypes: among others, fecal concentrations of acetate, butyrate, propionate and valerate are significantly higher in patients with IBS-D compared to patients with IBS-C. Finally, for each pathological subtype, the bacterial signatures identified could be correlated with a specific fecal concentration of SCFAs, fecal cytokine levels as well as stool consistency.
IBS SUBTYPES ACCORDING TO ROME IV
- IBS-D (associated with diarrhea)
- IBS-C (associated with constipation)
- IBS-M (mixed subtype)
- IBS-U (unclassified)
The pathophysiological mechanisms that fall under one subtype rather than another remain obscure, but the clinical differences foreshadow the existence of specific biological markers capable of guiding diagnosis and management.
CHRONIC CONSTIPATION: THE SEROTONIN PATHWAY (5-HT)
Although chronic constipation in adults is less often mentioned, it does impact quality of life. The disorder affects between 2% and 20% of the population depending on the study; it is frequently accompanied by intestinal dysbiosis and could involve hormone-mediated interactions. An international team has investigated serotonin, a key neurotransmitter of the gut-brain axis, which is thought to be involved in gastrointestinal motility. The concentration of serotonin, 95% of which is secreted by enterochromaffin cells, could be regulated by the intestinal microbiota via the expression of the serotonin transporter (SERT). This hypothesis was tested through fecal transplants from human subjects with chronic constipation and healthy individuals to mice whose microbiota was weakened by antibiotic therapy. The mice that received a transplant quickly displayed reduced gut peristalsis, abnormal defecation parameters, overexpression of SERT in the colon and reduced serotonin concentrations. Characterization of bacterial populations in these mice showed a depletion of Clostridium, Lactobacillus, Desulfovibrio and Methylobacterium genera and an enrichment of Bacteroides and Akkermansia genera. This reflects a marked dysbiosis, which, according to the researchers, could trigger positive regulation of SERT expression, and consequently increase the reuptake of the serotonin responsible for a reduction in intestinal motility.
13 Cao H, Liu X, An Y, et al. Dysbiosis contributes to chronic constipation development via regulation of serotonin transporter in the intestine. Sci Rep. 2017;7(1):10322.
14 Gargari G, Taverniti V, Gardana C, et al. Fecal Clostridiales distribution and short-chain fatty acids reflect bowel habits in irritable bowel syndrome. Environ Microbiol. 2018;20(9):3201-3213.
15 Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313(9):949-958.






