Microorganisms: key for human health
Small, invisible, but very much alive and highly sophisticated creatures, microorganisms are essential to life on Earth and to good health. How do they help us? How can we protect them? Why do some cause disease? Find out below.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information
About this article

Microorganisms: microscopic creatures with extraordinary powers
Microorganisms are living beings invisible to the naked eye, sometimes called “microbes” or “germs”. They’re generally made up of a single cell and can be found everywhere: from the depths of the ocean to the bottom of our gut, in the air, soil, plants, and rivers.
Microorganisms: tireless workers behind the scene
Microorganisms are essential to life on Earth thanks to their superpowers. These include a key role in the decomposition of plant and animal waste, or in carbon and nitrogen fixation. They’re essential links in the functioning of terrestrial ecosystems and key to the health of living beings.
Our bodies, too, form a true ecosystem, where populations of billions of “friendly” microorganisms live in harmony, providing us with a vast range of services. These populations are known as our “flora” or “ (sidenote: Microbiota Microbiota are the communities of microorganisms – mainly bacteria, but also viruses, fungi, and archaea – that colonize the human body. The type, number, and distribution of these microorganisms vary considerably from one area of the body to another. The gut microbiota – also known as the gut flora – contains the largest number of microorganisms. The gut microbiota is also the most studied. In humans, microbiota are also found in the vagina (vaginal microbiota), on the surface of the skin (skin microbiota), in the urinary tract (urinary microbiota) and respiratory tract (pulmonary microbiota), and in the ear-nose-throat area (ENT microbiota). These numerous microbiota interact with each other and take part in digestive, metabolic, immune, and neurological functions. ) ”. This type of microbial community can be found not only in animals and plants, but also in soils and the oceans1.
500 million The number of rhinoviruses (cause of the common cold) that could fit into a sphere the size of a pinhead.
1 billion The number of bacteria and viruses contained in 1 g of stool.
1 billion This is also the number of bacteria and fungi in 1 g of soil.
Microbiota are the communities of microorganisms – mainly bacteria, but also viruses, fungi, and archaea – that colonize the human body.
The gut microbiota – also known as the gut flora – contains the largest number of microorganisms. It is also the most studied.
In humans, we find microbiota :
A bacterium for every service rendered to mankind
- By fixing atmospheric nitrogen in the soil at the root of legumes, Rhizobium bacteria promote their growth while limiting the need for chemical fertilizers;
- Bacteria Lactobacillus acidophilus and Streptococcus thermophilus transform milk into yogurt;
- The fungus Penicillium roqueforti transforms curdled and fermented milk into blue cheese or Roquefort;
- Viruses called “phages” allow us to cure certain infections caused by antibiotic-resistant bacteria;
- The yeast Saccharomyces cerevisiae transforms sugars from wheat or barley into alcohol to make beer;
- Lastly, a collection of bacteria, fungi, and archaea allow water purification in wastewater treatment plants.
100 billion The number of bacteria in 1 g of dental plaque.
The saga of microorganisms
- 3.4 to 3.7 billion years ago: Appearance of the first bacteria and archaea (the first forms of life on Earth).
- 1665: English scientist Robert Hooke observes microorganisms (mold) under the microscope for the first time.
- 1674: Dutch draper Antonie van Leeuwenhoek observes bacteria under the microscope for the first time, naming them “animalcules”.
- 1838: German naturalist and zoologist Christian Gottfried Ehrenberg coins the term “bacteria”.
- 1857: Louis Pasteur demonstrates the role of bacteria in fermentation.
- 1882: Robert Koch discovers the bacillus responsible for tuberculosis.
- 1918: Spanish flu epidemic caused by the H1N1 virus (25 million deaths).
- 1930: First observation of a virus using an electron microscope.
- 1917: Félix d’Hérelle and Frederick Twort discover bacteriophages.
- 1929: Alexander Fleming discovers penicillin (antibiotic).
- 1977: Carl Woese discovers bacterial archaea.
- 1995: Craig Venter’s team sequences the first bacterial genome in its entirety.
- 2019: COVID-19 pandemic (SARS-CoV-2 virus).
Some definitions of microorganisms

Bacteria

Virus (including phages)

Protozoa
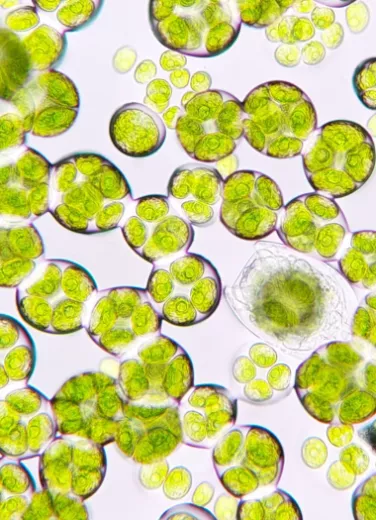
Microalgae

Fungi

Archaea
Together with viruses, bacteria are surely the microorganisms most familiar to the general public. Under the microscope, they come in a wide variety of shapes (rods, spheres, screws, etc.), and can be found everywhere: in plants, animals, humans, soil, the oceans, etc. Bacteria play an essential role in the decomposition of animal and plant organic matter. Fortunately for us, only a small number of them act as parasites or pathogens. Some spoil food, while others improve taste and preservation (fermentation). Most of the bacteria that live in symbiosis with humans are found in the digestive system (microbiota). In soils, Nitrobacter oxidizes nitrite into nitrate, while Methanobacterium transforms carbonate into methane. Propionibacterium transform milk lactose to give Emmental and Gruyère a nutty flavor, while certain non-pathogenic staphylococci contribute to cheese ripening and rind formation4.
Unfortunately, some bacteria are better known for their harmful effects on health. In our gut microbiota, most strains of Escherichia coli are harmless, but some can cause food poisoning. For example, the bacterium Shigella is responsible for a disease called shigellosis and caused 212,438 deaths worldwide in 2016. Vibrio cholerae is responsible for the world’s dreaded cholera epidemics and the 107,290 deaths recorded in 2016, generally in poor populations with no access to drinking water5. Other infamous examples are Clostridium tetani, which synthesizes a toxin responsible for tetanus, and Clostridioides difficile, an antibiotic-resistant bacterium that is the main cause of life-threatening nosocomial infectious diarrhea in adults5.
Within the large family of microorganisms, viruses are the smallest member. Their structure is extremely simple: a DNA or RNA molecule surrounded by proteins, which together form a “capsid”. One of the unusual features of viruses is that they’re completely dependent on a host cell. In other words, they have to penetrate the cell and hijack its machinery in order to replicate and infect new cells adjacent to it. This is how viruses that infect humans work (AIDS, colds, flu, etc.). Once released, the host cell dies, and the new viruses attack additional cells.
Despite their very poor reputation, not all viruses are pathogenic to humans, and some are even our friends. This is the case with viruses known as bacteriophages or phages (literally “bacteria eaters”), which infect only bacteria. Very useful for regulating certain bacterial populations, bacteriophages offer new therapeutic perspectives and are an alternative to antibiotics4. They include Siphoviridae, Myoviridae, and Podoviridae, which differ from “classic” viruses in that they have a tail that enables them to attach themselves to bacteria. Bacteriophages make up half of all known virus species4.
Taken together, all viral communities in the microbiota are known as the “virome”.
Less well known to the general public are protozoa, single cell microorganisms that come in a wide variety of forms, whether changing, like the amoeba, or fixed and complex, like the paramecium. They are mainly found in a range of moist environments, including freshwater, marine environments, and soil. They can move in “amoeboid” movements using cilia, or propel themselves using flagella. Some protozoa can infect plants and animals, including humans. This is the case with Plasmodium falciparum, infamous worldwide for causing severe forms of malaria, and dreaded on trips to certain countries4.
Microalgae can be found in fresh or sea water, particularly at the bottom of oceans, lakes, or rivers. They can sometimes develop in soils or on damp rocks, or in the coats of certain animals. They contain chlorophyll, which enables them to synthesize their own food from solar radiation. Diatoms are microalgae that sink to the seabed when they die. Their soft parts decay, while the silica cell wall sedimentates under the effect of water pressure4.
Phytoplankton are the microalgae found in seawater. Together with the bacteria and viruses that also live there, they make up the “marine microbiota”. This diverse population of microorganisms accounts for more than two-thirds of marine biomass. It positively influences the oceanic ecosystem and contributes to the health of the planet1.
Most fungi live in soils and on plants. There are three main groups of fungi: multicellular filamentous molds, macroscopic filamentous fungi, and single-celled microscopic yeasts4. In nature, molds and filamentous fungi participate in the cycling of carbon by developing long, branched filaments (mycelium) capable of decomposing plant matter. The largest known mycelium is located in Oregon (USA) and extends over 9.7 km2. In healthcare, Penicillium notatum was behind Alexander Fleming’s accidental discovery of penicillin in 1928, one of history’s great scientific breakthroughs6. In the agri-food industry, the domestication of certain filamentous fungi enables the production of cheeses. Penicillium roqueforti is used to ripen blue cheeses, while the Penicillium camemberti species complex is used to manufacture soft cheeses such as Camembert and Brie6. Yeasts like Saccharomyces multiply by budding off a daughter cell from the original parent cell. The species Saccharomyces cerevisiae is used in the production of wine and beer6.
Some fungi are plant parasites that cause diseases such as mildew or scab. Only a small number of fungi affect human health. These include ringworm, thrush, and the yeast Candida albicans, which causes candidiasis4.
Long classified as bacteria, which they closely resemble, archaea are single cell microorganisms that sometimes form filaments or clusters. Research in the 1970s showed them to be evolutionarily distinct from bacteria. They share common features with eukaryotic cells (such as human cells), which have a more complex structure than prokaryotic bacteria. Archaea can live in extreme environments, such as high pressures or salinity levels, or very low or very high temperatures (hot springs, geysers, Antarctic ice, etc.)4. Halobacterium or Halococcus live in salt lakes and have a red or yellow color due to their pigments, while Pyrobaculum reproduce underground, in oil reservoirs, at over 100°C.

Love your microbes and they’ll love you in return
If you thought microbes were only fit to be eliminated, by now you can see you were wrong. The vast majority of microbes are essential to human life and activity. They’re also essential to the functioning of our body and to good health.
Mutually beneficial value exchange3, 7, 8
Our bodies are home to a varied multitude of “commensal” microorganisms – as opposed to pathogenic microorganisms – with which we have a truly symbiotic relationship. In exchange for food and shelter, these microbes provide us with invaluable services.
Some surprising numbers
5,000 billion billion billion (i.e. 5 x 1030)
The number of bacteria and archaea living on the planet.
They’re by far the most common form of life on Earth.
100 million light-years
The distance that would be covered if the 1031 viruses living on Earth were put in a line.
Our microbiome contains 50 to 150 times more types of gene than the cells of our body. The microbiome is in reality a “second genome”.3
The human body contains 10 times as many bacteria as cells.2
In the gut, bacteria in the microbiota feed on dietary fiber – which we’re unable to break down – and release essential compounds known as “ (sidenote: Short chain fatty acids (SCFA) Short chain fatty acids (SCFA) are a source of energy (fuel) for an individual’s cells. They interact with the immune system and are involved in communication between the intestine and the brain. Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. ) ”. These molecules nourish gut cells, contributing to their growth and differentiation, and reinforcing their barrier function. Microbes also synthesize useful bioactive substances, such as amino acids and vitamins (K2, B5, B6, etc.).
They also play a role in the maturation of immune cells, particularly numerous in the gut wall, and, by occupying the terrain and synthesizing certain antibacterial proteins called bacteriocins, protect us against the proliferation of pathogenic microorganisms. Lastly, they synthesize (sidenote: Metabolites Small molecules produced during cellular or bacterial metabolism. For example, short-chain fatty acids are metabolites produced by intestinal microbiota during fermentation of non-digestible complex carbohydrates (fibers, etc.). Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. Lamichhane S, Sen P, Dickens AM, et al An overview of metabolomics data analysis: current tools and future perspectives. Comprehensive analytical chemistry. 2018 ; 82: 387-413 ) capable of regulating some of our physiological functions, notably our immune and neuronal functions. For example, the microbiota and the brain are in permanent communication via the so-called microbiota-gut-brain axis.
The gut-brain axis : what is the role of the microbiota?
How to pamper your microbes 3, 7, 8
The health of our microbiota depends on many factors: genetics, age, living environment, mode of birth, etc. But the most powerful modulator of the gut microbiota remains our diet. A “healthy” microbiota, i.e. one that is rich and diversified, requires a diet that includes a sufficient variety of plants (fruits, vegetables, oilseeds, whole grains, legumes, etc., which provide the right “substrates”, or food, for the microorganisms), as well as live bacteria (fermented foods such as sauerkraut, kombucha, kefir, etc.).
Our diet should not include too many harmful foods, such as those containing emulsifiers and sweeteners.
Cutting back on certain medications (antibiotics, antacids, laxatives, anxiolytics, etc.), moderating alcohol and tobacco consumption, and regular physical activity are also excellent ways to promote a healthy microbiota.
When microbes go bad, our body pays the price
Microbes are responsible for a multitude of infectious diseases: the rhinovirus for colds, the SARS-CoV-2 virus for COVID-19, the Salmonella bacterium for gastroenteritis, the Candida fungus for candidiasis, etc. Fortunately, we now have antimicrobials (antibiotics, antivirals, antifungals, etc.) that can treat the majority of infections caused by microorganisms.
Beware of antimicrobial resistance in microorganisms
In recent years, the overuse of these treatments has led to the proliferation of bacteria, viruses, and fungi that have become resistant to them. For example, certain pathogenic bacteria no longer respond to any antibiotic treatment. These are known as “multi-resistant” or “superbug” bacteria. As a result, certain illnesses that used to be treatable (urinary tract infections, sexually transmitted or nosocomial infections, diarrhea, tuberculosis, etc.) can now be difficult or impossible to treat.9
Recognized as a public health issue by the WHO, antimicrobial resistance may kill up to 10 million people per year by 2050 (as many as cancer).10 The WHO recommends limiting the use of antimicrobials, particularly antibiotics, in livestock farming, human healthcare, and agriculture, but above all calls for new, more effective treatments for infections.
La Semaine mondiale de sensibilisation à la résistance aux antimicrobiens (en anglais : WAAW pour World AMR Awareness Week) est célébrée chaque année du 18 au 24 novembre. En 2023, le thème retenu est « Prévenir la résistance aux antimicrobiens ensemble », comme en 2022. En effet, cette résistance représente une menace pour les êtres humains, mais aussi les animaux, les plantes et l'environnement.
L’objectif de cette campagne est donc à la fois de sensibiliser à la résistance aux antimicrobiens et de promouvoir les meilleures pratiques, selon le concept « Une seule santé », ou « One health », auprès de toutes les parties prenantes (grand public, médecins, vétérinaires, éleveurs et agriculteurs, décideurs…) afin de réduire l'apparition et la propagation d'infections résistantes.
Imbalances: the breeding ground for lifestyle diseases 3, 5, 8
Microorganisms aren’t only responsible for infectious diseases. Did you know that microorganisms also play a role in obesity, diabetes, osteoporosis, cancer, vascular diseases, and neurodegenerative diseases (Parkinson’s, Alzheimer’s, etc.) ?
Studies show that people suffering from these illnesses have an imbalance in their microbiota known as “ (sidenote: Dysbiosis Generally defined as an alteration in the composition and function of the microbiota caused by a combination of environmental and individual-specific factors. Levy M, Kolodziejczyk AA, Thaiss CA, et al. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17(4):219-232. ) ”. Dysbiosis is characterized by a loss of richness and diversity in microbial populations, particularly in the gut. Numerous studies have shown that such imbalances can have a negative impact on the way our body functions, and can contribute to the onset or aggravation of disease.
The data currently available fail to give a precise answer as to whether dysbiosis causes disease or disease causes dysbiosis. However, studies suggest that it may be possible to maintain good health by ensuring the microbiota is rich and diversified, i.e. “healthy”, or by rebalancing it.
Have you heard of dysbiosis
Modulate the microbiota to prevent or even cure disease!
There are several ways to positively modulate the gut microbiota in cases of dysbiosis or disease 3, 7 :
- Diet and lifestyle (see above);
- Prebiotics (inulin, galactooligosaccharides [GOS], fructooligosaccharides [FOS], and lactulose): these compounds are capable of specifically feeding groups of beneficial bacteria, such as Bifidobacterium and Lactobacillus, thus encouraging their proliferation11;
- Probiotics (specific strains of live bacteria or yeast with proven health benefits): to date, scientific evidence of their efficacy is limited to childhood diarrhea, antibiotic-associated diarrhea, certain inflammatory bowel diseases, and necrotizing enterocolitis, but their therapeutic potential is the subject of much research11.
- Bioactive (sidenote: Metabolites Small molecules produced during cellular or bacterial metabolism. For example, short-chain fatty acids are metabolites produced by intestinal microbiota during fermentation of non-digestible complex carbohydrates (fibers, etc.). Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. Lamichhane S, Sen P, Dickens AM, et al An overview of metabolomics data analysis: current tools and future perspectives. Comprehensive analytical chemistry. 2018 ; 82: 387-413 ) : have the ability to modulate the physiology of target microorganisms;
- Fecal microbiota transplantation (FMT): involves transferring the gut microbiota of a healthy person into the gut of a sick person. For example, FMT has shown particularly solid results (90% cure rate) for Clostridium difficile infections12 but may also be useful for alleviating the symptoms of autism 13.

The microbial world: an infinite source of therapeutic possibilities
Microorganisms are a valuable field of research for scientists. For example, in order to better combat bacterial resistance to antibiotics and develop monitoring tools, scientists need a better understanding of how bacteria exchange genes, how they acquire antimicrobial resistance, and the pathways by which this resistance circulates between the environment, humans, and animals10.
High-resolution genomics and metagenomics techniques, widely used in human microbiota studies, are powerful tools for exploring microbial dynamics.
Microbiota at the crossroads of research
An ever-increasing number of studies seek to improve our understanding of how microorganisms in the microbiota interact with humans and contribute to the proper functioning of human cells, and to reveal which microbial profiles are most beneficial to health, and which modifications contribute to disease3.
The ultimate goal is to identify new therapeutic avenues and new probiotic bacteria that will make it possible to modulate the microbiota and thus manage certain acute and chronic illnesses more effectively.
A number of promising avenues
- It may be possible to use certain substances naturally produced by bacteria, e.g. bacteriocins, to develop new treatments which can eliminate pathogenic microorganisms or slow down their development. Furthermore, other molecules metabolized by bacteria, such as (sidenote: Short chain fatty acids (SCFA) Short chain fatty acids (SCFA) are a source of energy (fuel) for an individual’s cells. They interact with the immune system and are involved in communication between the intestine and the brain. Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. ) may be useful for their multiple health benefits, including anti-inflammatory and anti-cancer effects.
- Genetically modulating bacteria such as Escherichia coli may enable them to produce different types of molecule with a medical interest, some designed to positively modulate the microbiota in the event of antibiotic-induced dysbiosis, others acting as a vaccine to combat Vibrio cholerae (the bacterium responsible for cholera), and still others capable of specifically killing pathogens such as Pseudomonas aeruginosa, a bacterium that wreaks havoc on the immunocompromised.
- Lastly, it may be possible to use bacteriophages to precisely target antibiotic-resistant bacteria in cases of infection, potentially providing a powerful alternative to antibiotics.
As you can see, although microorganisms are invisible and have a bad reputation, they deserve our full respect and attention, since they’re essential to our lives.
Much mystery still surrounds the communities they form, their interactions with the environment, and the role they play in our organism, but not a day goes by without a new study showing the importance of having them on our side, and thus of strengthening our symbiosis with them.
























