Postoperative pain: a question of gut microbiota?
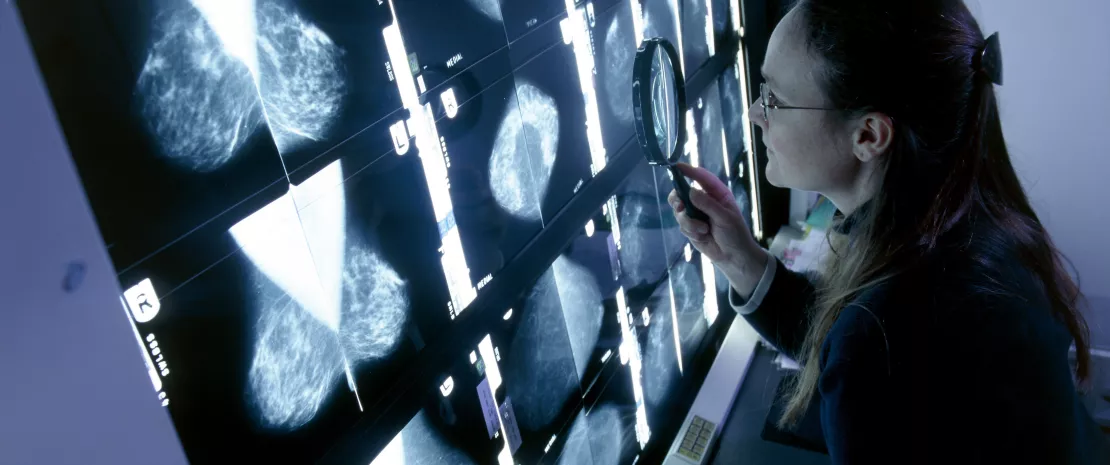
While previous work has linked the diversity and composition of the gut microbiota to postoperative pain after wrist surgery, a team has now identified for the first time bacteria associated with the presence or absence of persistent post-surgical pain following breast cancer surgery.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Persistent post-surgical pain (or (sidenote: Persistent post-surgical pain (PPSP) Pain which continues after a surgical operation in a significant form for at least three months, and is not related to pre-existing painful conditions ) ) is as common as it is underestimated: it affects millions of patients worldwide. Predisposing factors include the type of surgery. For example, in the case of breast cancer, 80% of women whose surgery includes axillary lymph node clearance suffer from PPSP.
Previous studies have implicated the gut microbiota in postoperative pain. However, the mechanisms remained unclear: gut dysbiosis could induce an imbalance in the production of microbial metabolites, and play a role in the development of PPSP via
(sidenote:
Gut-brain axis
Two-way communication network between the gut and the brain, which allows the gut and brain to communicate via three different pathways:
1. the neuronal pathway (neurons), mainly via the vagus nerve and the enteric nervous system,
2. the endocrine pathway, by secreting hormones such as cortisol, adrenaline and serotonin
3. the immune system pathway, by modulating cytokines
The gut-brain axis influences our behavior, cognition (memory), emotions, moods, desires, perception... and pain, among other things.
)
.
To find out more, Irish researchers at University College Cork 1 conducted a prospective observational study of adult patients undergoing surgery for breast cancer (excluding axillary clearance or reconstructive surgery, which are very painful). Their aim was to determine whether the composition of the gut microbiota was associated with the incidence and extent of PPSP in this cohort of patients.
2.3 million In 2022, there were 2.3 million women diagnosed with breast cancer and 670,000 deaths globally ²
most common cancer Breast cancer was the most common cancer in women in 157 countries out of 185 in 2022 ²
Approximately 99% des cancers du sein surviennent chez les femmes, contre 0,5 à 1 % chez les hommes ²
Less alpha diversity
Twelve weeks after the operation, 21 patients (51.2%) reported no pain, while 20 (48.8%) reported persistent pain. This difference seemed to be linked to the diversity of their gut microbiota: a lower (sidenote: Alpha diversity Number of species coexisting in a given environment ) (3 measures: richness, Shannon index and Simpson index) was observed in patients reporting severe pain 1 hour after surgery and 12 weeks later, compared to those reporting mild pain. On the other hand, there was no difference in (sidenote: Beta diversity Rate of variation in species composition, calculated by comparing the number of unique taxa in each ecosystem ) .
Bacteria associated with the presence or absence of pain
But above all, the team highlighted stark differences in the composition of the gut microbiota corresponding to pain, with increased presences of:
- Bifidobacterium longum and Faecalibacterium prausnitzii in women who reported no pain 12 weeks after surgery
- Megamonas hypermegale, Bacteroides pectinophilus, Ruminococcus bromii and Roseburia hominis in women with PSPP.
These results seem to support those of previous studies: reduction in the relative abundance of Faecalibacterium prausnitzii in patients with fibromyalgia; reduction of pain after the administration of Bifidobacterium longum in a rat model with arthritis. There is one exception, however: Roseburia hominis reduced visceral hypersensitivity in rats, while it was associated with the presence of PPSP in this study.
While these relationships between microbiota and PSPP are a first, the authors caution that they are only correlations and not causal links.












