Cancer immunotherapy: no prior antibiotic treatment
Gut dysbiosis caused by the prior use of broad-spectrum antibiotics could impact the efficacy of cancer immunotherapy, in turn leading to a decrease in overall patient survival.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
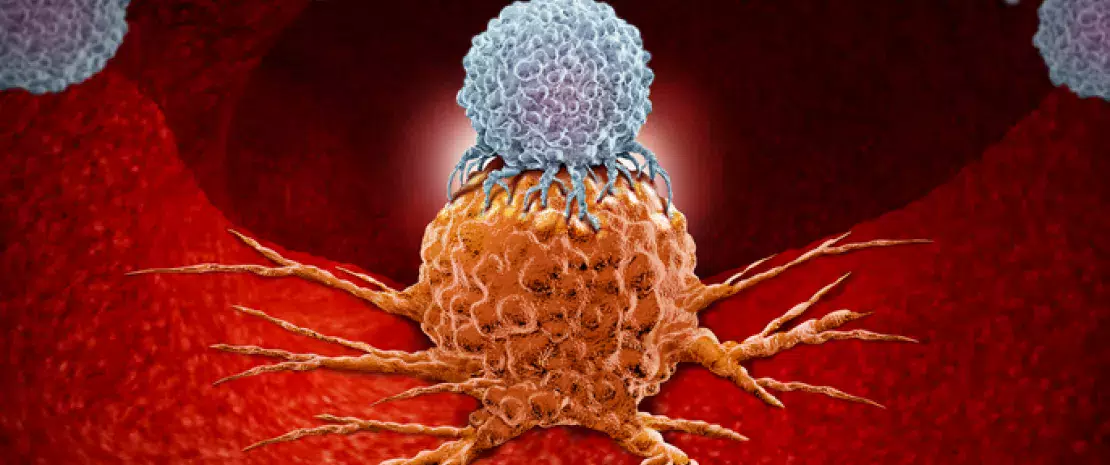
Immune checkpoint inhibitor (ICI) therapy is a form of immunotherapy that provides a new therapeutic option against some tumors, such as melanoma and non-small-cell lung cancer (NSCLC). Despite its efficacy, only a small number of patients can benefit from it. That is why it is important to better anticipate the response to treatment and improve routine prescription guidelines. To this end, a team of researchers investigated if the time of administration of broad-spectrum antibiotics (ATB) which are mainly used to treat respiratory infections–either prior or concomitantly to ICI– could have an impact on the treatment efficacy through gut microbiota modulation.
Patient survival decreased from 26 to 2 months
This prospective cohort study, conducted at 2 teaching hospitals, included 196 patients (137 male and 59 female, average age: 68 years) with cancer (119 NSCLC, 38 melanoma and 39 other types of cancer) who received ICI therapy for more than three years. The results indicate that antibiotic therapy given in the 30 days prior to ICI therapy (pATB, i.e prior antibiotics) clearly decreases overall patient survival, regardless of the type of cancer (2 months for patients who received pATB vs. 26 months for those who did not receive any prior antibiotic treatment). The percentage of tumors refractory to therapy is also considerably higher in patients who received pATB (81% vs. 44%). In conclusion, the time of administration of antibiotics seems crucial: while it does not have any negative impact if given concomitantly to ICI therapy, it worsens the prognosis when it is administered previously.
Understanding the role of the gut microbiota
The authors are aware that their results are limited by the small cohort size and by the lack of correlation analysis between antibiotic therapy and composition of the patients’ microbiota. But they are in line with results from previous studies indicating that gut dysbiosis is associated to a poor response to ICI therapy against cancer. One possible explanation is that the use of antibiotics could lead to long-lasting disruptions in the gut ecosystem which would then jeopardize the efficacy of T cells against cancer. However, this is still an imprecise hypothesis, and mechanistic studies should be carried out as soon as possible in order to understand how gut microbiota alterations induced by prior antibiotic use negatively impact the efficacy of ICI therapy.






