Oral microbiota transplantation: a ray of hope for preventing chemotherapy-induced mucositis?
A pilot study 1 on a female infant with neuroblastoma shows that transplantation of the mother’s oral microbiota could effectively prevent chemotherapy-induced mucositis.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
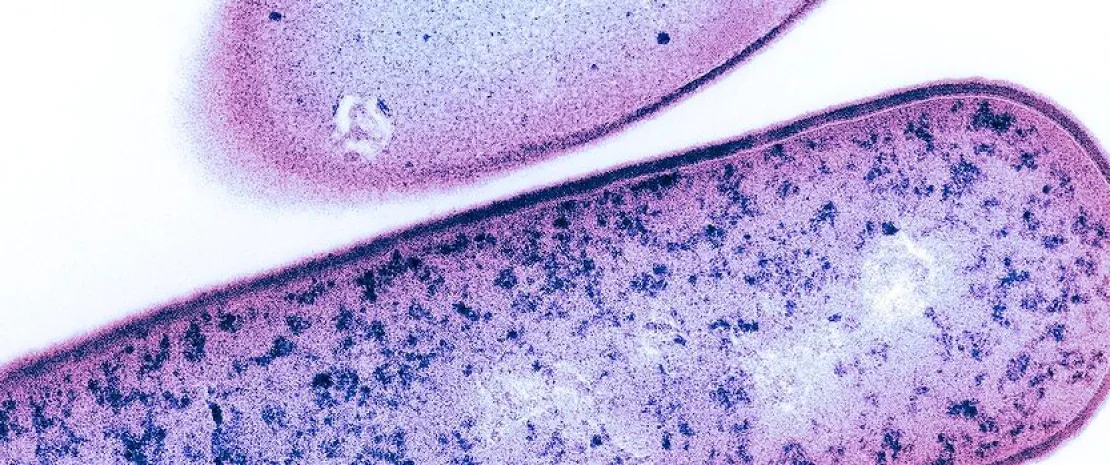
(sidenote: Oral mucositis Acute, painful inflammation of the oral mucosa, often induced by anti-cancer treatments such as chemotherapy and radiotherapy. Symptoms include redness, pain, and ulceration, and can be accompanied by dry mouth, altered taste, and difficulty in eating. It can lead to malnutrition, dehydration, and reduced quality of life. Treatment is symptomatic and aims at relieving pain, promoting healing, and preventing infection. Explore Cleveland Clinic ) is a common side-effect of chemotherapy and radiotherapy. It is characterized by inflammation of the oral and intestinal mucosa.
The result is lower quality of life for patients, poorer compliance with treatment, feeding difficulties, and complications that are all the more serious when the patient is frail. Since current therapies only treat symptoms, modulating the oral microbiota seems to be a promising new approach.
Following on from work suggesting a link between oral microbiota and the development of chemotherapy-induced mucositis, the publication at the end of 2024 of a pediatric clinical case has increased our hopes.
Oral mucositis is diagnosed in more than 70% of patients after hematopoietic cell transplantation and in 40% of patients receiving chemotherapy at standard doses.
Decision and transplantation protocol
The story relates to a six-month-old Russian girl, diagnosed at the age of four months as suffering from a retroperitoneal neuroblastoma with multiple metastases. Chemotherapy was rapidly complicated by various side effects, including severe oral mucositis, rapid weight loss, and C. difficile infection.
The doctors decided to perform a transplant of the healthy 33-year-old mother’s oral microbiota. The donation samples were spread out over the day (nine samples of 1.5 mL), away from meals and tooth brushing.
Oral microbiota and chronic conditions
Oral transplantation
During each of the following three cycles of chemotherapy (the dosage of which was reduced), the infant received her mother’s saliva in her mouth (13.5 mL per day for 10 days) some thirty minutes after breast-feeding.
After six chemotherapy cycles, the patient underwent a complete resection of a retroperitoneal tumor along with right-sided adrenalectomy, followed by high-dose chemotherapy with subsequent autologous hematopoietic cell transplantation (auto-HCT). A final oral transplant of maternal saliva was performed prior to the auto-HCT.
Effects on mucositis
Oral microbiota transplantation effectively prevented the development of mucositis following three new cycles of chemotherapy, and only grade 1 oral mucositis developed after auto-HCT. In all parts of the mouth, there was a decreased abundance of bacteria from the Staphyloccaceae, Micrococcaceae, and Xanthomonadaceae families. Conversely, there was an increase in the relative abundance of Streptococcaceae and certain other bacterial taxa.
Maternal saliva transplantation thus appears to have prevented further severe mucositis in the patient, and to have been accompanied by a change in oral microbiota composition. No adverse events due to the transplantation of maternal saliva were noted.
Although it is only one case, the pilot clinical study described here paves the way for possible oral microbiota transplants to reduce the risk of mucositis during chemotherapy. At the very least, it highlights the possibility, safety, and efficacy of transplanting oral microbiota from a healthy donor to a neuroblastoma patient to prevent chemotherapy-induced oral mucositis.










