Microbiota transplant and type 1 diabetes mellitus: a trial in humans
Fecal microbiota transplantation is accompanied by changes in microbial metabolites and T cells involved in autoimmunity and may preserve residual function of pancreatic β-cells in type 1 diabetes mellitus.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
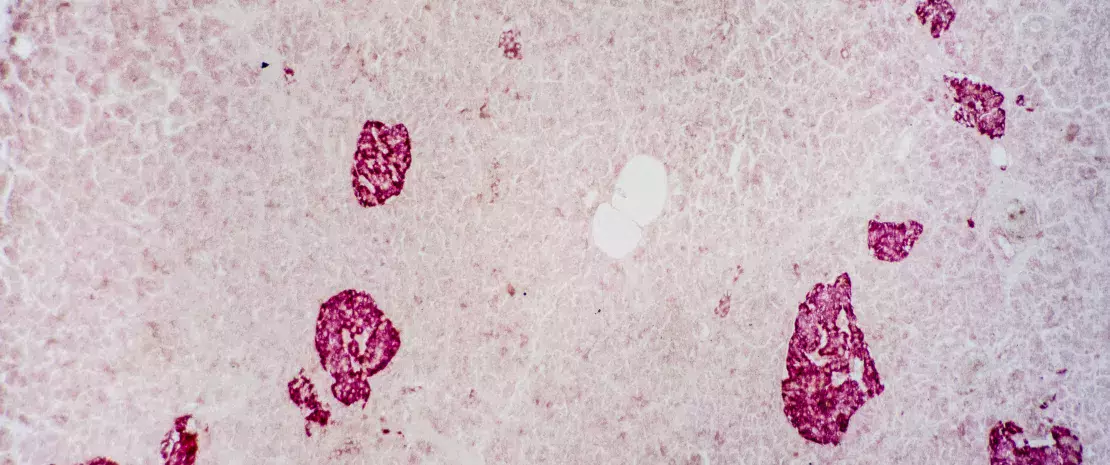
Type 1 diabetes mellitus (T1DM) is an autoimmune disease that leads to the destruction of pancreatic β-cells. Studies in mice suggest that interactions between the gut microbiota and the innate immune system are involved in the development of the disease, the progression of which may be slowed by fecal microbiota transplantation (FMT).
Autologous versus allogenic transplantation
In a randomized controlled trial, patients recently diagnosed with T1DM received three FMTs by nasoduodenal tube at 0, 2 and 4 months, either from their own feces (autologous FMT, n=10) or from the feces of healthy donors (allogenic FMT, n=10). In the year following the first FMT, the researchers evaluated residual β-cell function (via C-peptide release in response to a test meal), as well as metabolic, immune and microbiota changes induced by the two types of FMT.
Pancreatic function preserved
Contrary to the researchers’ expectations, β-cell function was preserved in the autologous group one year after the first FMT. β-cell function deteriorated in the allogenic group, however, although less than in (sidenote: Overgaard AJ, Weir JM, Jayawardana K, et al. Plasma lipid species at type 1 diabetes onset predict residual beta-cell function after 6 months. Metabolomics 2018;14:158; Lachin JM, McGee PL, Greenbaum CJ, et al. Sample size requirements for studies of treatment effects on beta-cell function in newly diagnosed type 1 diabetes. PLoS One 2011;6:e26471 ) . According to the researchers, the benefits of FMT may be more pronounced and long-lasting where immunological compatibility between donor and host is high.
Desulfovibrio piger involved?
Changes in the microbiota were found to be associated with certain metabolic and immune changes. In the duodenum, the presence of Prevotella spp. was inversely correlated with residual β-cell function. In the colon, Desulfovibrio piger became significantly more abundant following autologous FMT only. Its abundance was associated with improved residual β-cell function and increased levels of plasma 1-arachidonoyl-GPC (A-GPC), a microbial metabolite associated with increased C-peptide production. In addition, the abundance of D. piger was negatively correlated with levels of certain T cells involved in autoimmunity. What was the significance according to the authors? D. piger may inhibit autoimmunity by suppressing these T cells via the production of A-GPC. From the multiple correlations found, the researchers have identified mechanistic leads that will need to be further investigated to clarify the effects of FMT on T1DM. They have also newly identified the therapeutic potential of certain bacterial species.






