Itchiness: learning about the mechanism of action of S.aureus from scratch
The aim of this study was to provide relief to patients suffering from pruritus through a better understanding of why S. aureus causes an irresistible urge to scratch.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Although seemingly harmless, itchy skin can be difficult to live with if it lasts long enough to disrupt daily life or even sleep, or if it results in scratching lesions. Pruritus is associated with a dysbiosis of the skin microbiota and is a major factor in the reduced quality of life of patients suffering from skin diseases (atopic dermatitis, psoriasis, etc.). But what causes pruritus? The results of a study published in 2024 show that opportunistic pathogen Staphylococcus aureus triggers itching by activating dedicated sensory neurons, the
(sidenote:
Pruriceptors
Pruriceptors are the sensory neurons that mediate itch and a desire to scratch.
Pruriceptor nerve endings are mainly found in the epidermis, unlike nociceptors, which innervate both skin and deeper tissues.
Source: https://www.has-sante.fr/jcms/c_2579446/fr/zontivity-vorapaxar-antiagregant-plaquettaire
)
.
From S. aureus to scratching
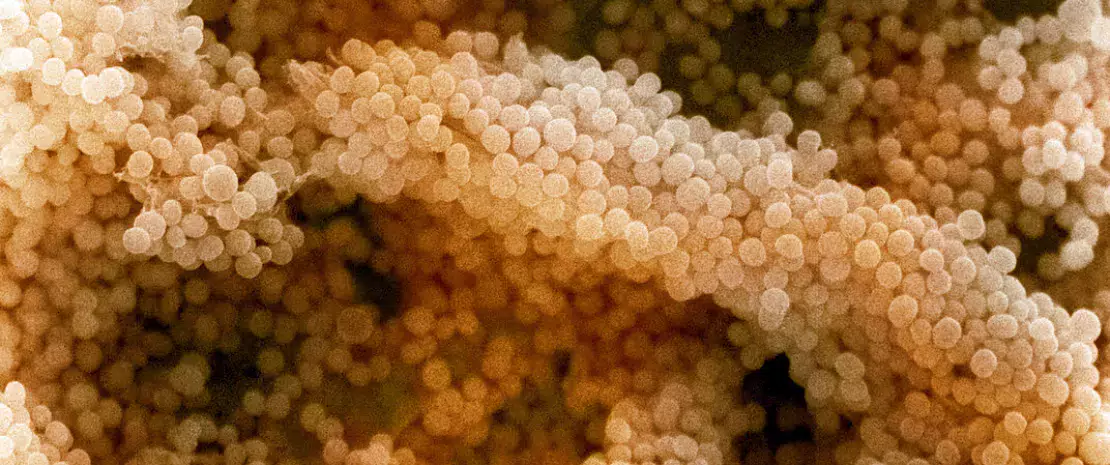
To better understand the mechanisms involved, researchers conducted an extensive series of experiments in vivo (mice) and in vitro (skin and neuron samples, including human neurons). It all starts with the S. aureus bacterium, which is capable of producing proteins that facilitate the colonization and invasion of host tissues. These include various toxins (α-hemolysin and phenol-soluble modulins) and around ten proteases. One of these bacterial enzymes, protease V8, is a critical factor in evoking itch. How? Protease V8 induces itch in mice and humans by stimulating pruriceptors via the activation of this neuron’s PAR1 subcutaneous receptor. The bacterium may take advantage of the itch it causes, since scratching potentially enables it to spread to other areas of the body, or even other hosts, while the skin lesions induced may allow the pathogen to penetrate deeper into the injured layer of skin.
90 % of AD lesions are colonized with S. aureus, which is thought to be a trigger of inflammation.
Other mechanisms also considered
As for the toxins secreted by S. aureus, the study showed that α-hemolysin and phenol-soluble modulins are also capable of activating sensory neurons and triggering itch. However, S. aureus bacteria that are unable to produce these toxins still trigger itching in mice, suggesting that bacterial toxin levels alone are not sufficient to trigger itch.
Of course, there are many other protease-secreting bacteria, whose role should be investigated: Staphylococcus epidermidis produces the protease EcpA, which causes skin lesions in patients with atopic dermatitis; while Streptococcus pyogenes produces the protease SpeB, which is involved in skin infections. And what can be said for fungi, viruses and parasites, whose potential contribution of itch-provoking proteases remains unknown?
Relieving patients
These initial results may one day help to relieve patients suffering from chronic skin itching, including cases of atopic dermatitis. This may be achieved by targeting protease V8, for example. Another promising option is the PAR1 receptor, the inhibition of which (e.g. using
(sidenote:
Vorapaxar
Vorapaxaris a PAR1 antagonist. It inhibits the thrombin action on the PAR1 receptor, preventing platelet aggregation via this pathway. In the United States, it has been approved by the Food and Drug Administration (FDA) as a drug that reduces the risk of thrombotic cardiovascular events. In France, its medical benefits as an antiplatelet agent have been judged insufficient.
Source: https://www.has-sante.fr/jcms/c_2579446/fr/zontivity-vorapaxar-antiagregant-plaquettaire
)
) is sufficient to reduce (but not entirely eliminate) itching, making it a prime target for the development of a new generation of topical creams.











