Chronic inflammatory bowel diseases
Recent studies on the interactions between immunity and microbiota shed a new light on the complex etiology of chronic inflammatory bowel diseases. Several mechanisms have been described and genetic predispositions have been identified thanks to animal models. But many factors remain unknown, especially those that trigger these diseases.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
About this article
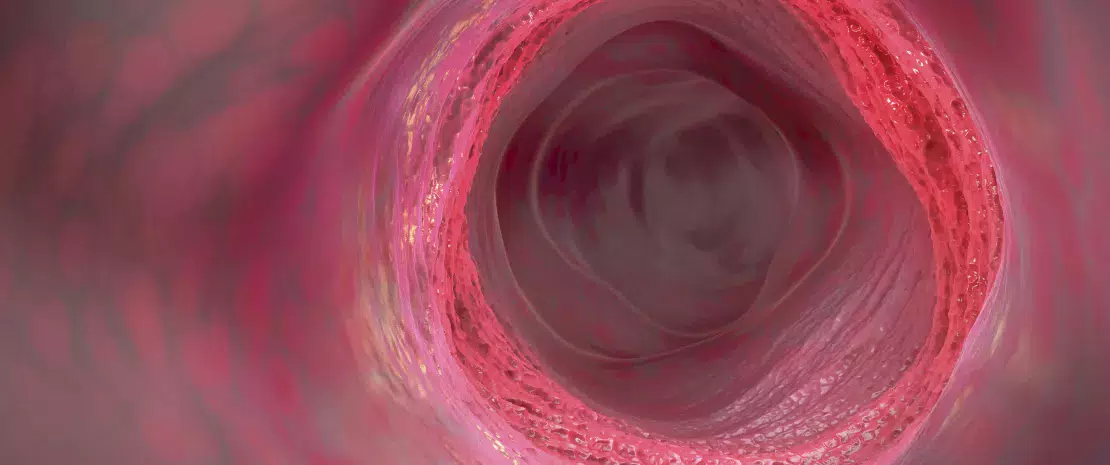
It has now been proven that dysbiosis and CIBD go hand in hand. Thinner or disrupted gut mucosa promotes the invasion of pathogenic bacteria into the epithelium, the mobilization of innate immune cells (macrophages and monocytes) and the production of TNF-α, inducing a chronic inflammatory state. Tolerance to commensal bacteria would be compromised, thus maintaining–or even worsening–the dysbiosis, and as a result the persistence of the inflammatory processes. The proof of this is that germ-free animal models for CIBD do not spontaneously develop the disease.
SEVERAL POSSIBLE ALTERATIONS
Underlying interactions between immunity and gut microbiota have been described in mouse models: the presence of bacteria from the Lachnospiraceae family seems to promote epithelial infiltration of proinflammatory monocytes and macrophages, which is alleviated by the administration of vancomycin. Moreover, hydrogen peroxide-producing bacteria in the colon could induce oxidative stress harmful to the intestinal mucosa. In a mouse model of ulcerative colitis, colonization of the intestines by a human microbiota with low content of Firmicutes led to the induction of proinflammatory Th17. Similar results were found in Crohn’s disease: in mice colonized by a patient’s microbiota, the activation of proinflammatory responses was observed, contrary to what occurs in mice colonized by other healthy mice/donors. Finally, in subjects with CIBD, the abundance of Faecalibacterium prausnitzii is reduced.5 This prominent species of the fecal microbiota in healthy individuals (5 to 20%) produces butyrate, has anti-inflammatory properties thanks to part of its microbial anti-inflammatory molecule (MAM) and is necessary to the good functioning of intestinal cells.10
THE WEIGHT OF GENETICS
Genetic predispositions involving dysfunctions of the innate response were also described . For instance, mutations of genes related to autophagy or to the identification of fungi by dendritic cells seem to predispose to Crohn’s disease. In this pathology, the mutation of the gene encoding NOD2 protein opens another avenue of research: this intracellular receptor of intestinal innate immune cells is able to bind many bacterial components (peptidoglycan, flagellin…) and activate the inflammatory immune cascade. However, the deactivation of the NOD2 gene alone is not enough to trigger the spontaneous onset of the disease in rodents. This suggests that commensal bacteria play a joint role. The effects of this mutation differ between animal models: in a chemically-induced colitis model, the mutation of the NOD2 protein has a protective role. Thus, the recurring question remains: is the inflammation the cause or the consequence of dysbiosis? Researchers have yet to reach a conclusion.






