Use of probiotics
Treatment with strains of living beneficial bacteria was long considered the safest and most sustainable approach against IBD. Although some of them seem effective to treat UC, studies regarding their use against CD are still inconclusive.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
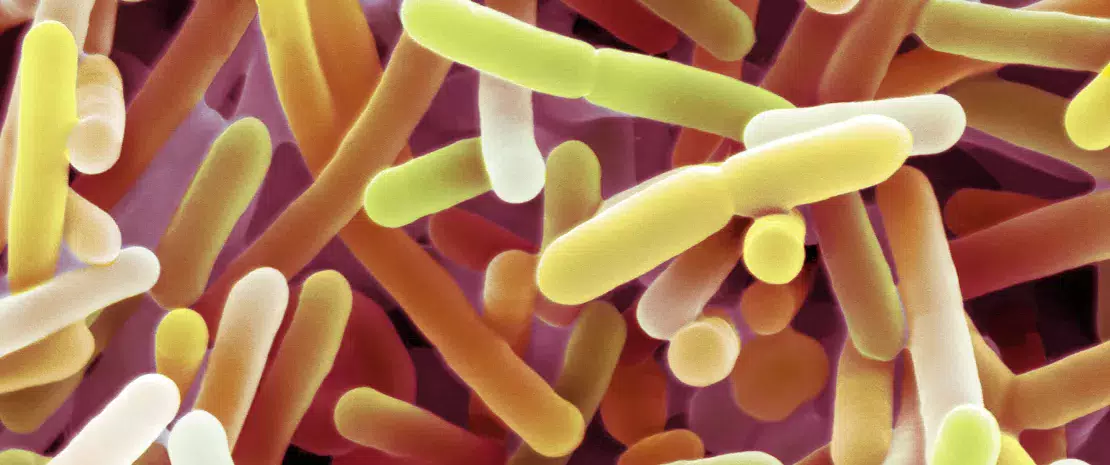
Scanning electron micrograph (SEM) of Bifidobacterium sp. Gram-positive anaerobic bacteria.
About this article
Probiotics are living microorganisms which, when ingested in adequate quantities, provide health benefits. Several mechanisms of action might underlie the beneficial effects of probiotics in IBD: inducing changes in the gut microbiota composition thus reducing gut dysbiosis; regulating metabolic activity of the gut microbiota; eliminating pro-inflammatory processes; and immunomodulation.12
Contrasted results depending on the disease
In UC, the efficacy of probiotics containing one and only strain (from the E. coli species), as well as milk fermented with Bifidobacterium, in inducing disease remission was comparable to that of standard anti-inflammatory treatments (mesalazine).12 Different combinations of bacterial strains were also tested, but with no effect on disease remission, with one exception: a cocktail of 8 different strains15 induced a significant reduction in UC symptoms,13,16 (rectal bleeding and stool frequency) and a study proved its efficacy in maintaining remission. This same cocktail also seems to be efficient in patients with pouchitis: it prevents inflammatory flares arising from coloproctectomy and maintains remission,17,18 however, probiotics have not shown to be useful in CD so far. Results from the rare studies performed are weak and inconclusive, including with strains that have proven to be efficient against UC and pouchitis.12,15
Further investigations
Heterogeneity of non-clinical and clinical results could be at least partially attributed to factors related to the host (age, gender, diet, disease location, severity, family history of IBD) and the probiotic preparations that were used (type of strain, concentration, mode of administration, potential colonization, and strain survival rate). Other factors, such as dose and duration of probiotics administration, are also supposed to play a primary role in the success of this therapeutic approach, whose adverse effects are minimal, or even nonexistent.12
SANITARY AND DIETARY RULES
- Excess in energy and/or macronutrients intake (saturated fat? refined sugar?) seem to increase gut inflammation, while several micronutrients could modulate it: vitamins A, C, E and D, folic acid, beta-carotene, trace elements (zinc, selenium, manganese and iron).2
- Since there are no existing dietary recommendations specific to IBD, patients are advised to avoid food which might worsen symptoms (high-fiber foods during flares, caffeine, alcohol, excess fatty foods, etc.).2
- The specific carbohydrate diet (SCD) which limits complex carbs and eliminates simple sugars, the low FODMAP diet (no fermentable sugars) and the Mediterranean diet have shown anti-inflammatory properties and may induce improvement under certain conditions. However, elimination diets are controversial because of a nutrition imbalance risk.2
- No smoking.2
15 Lactobacillus paracasei, L. plantarum, L. acidophilus, L. delbrueckii, Bifidobacterium longum, B. breve, B. infantis, Streptococcus thermophilus.






