Phage therapy for multidrug-resistant infections?
With the emergence of antibiotic resistance, bacteriophages are making a grand comeback. These viruses from the intestinal microbiota could eventually be used to provide more targeted treatment for multidrug-resistant infections, to give just one example. An article in Nature Reviews Gastroenterology & Hepatology looks at the history, future, and challenges of phage therapy.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
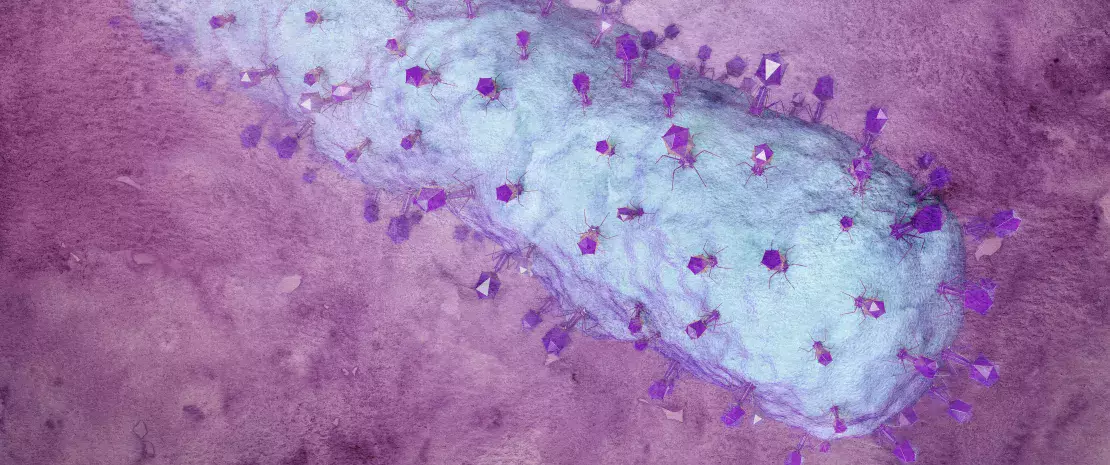
Bacteriophages, or simply “phages,” are the most abundant and varied biological agent on Earth. The natural predators of bacteria, they are ubiquitous in the earth, oceans... and the human intestinal microbiota, where they are the dominant type of virus. Intestinal bacterial dysbiosis, which is associated with gastrointestinal disorders such as Crohn's disease and Irritable Bowel Syndrome, goes hand in hand with compositional changes in the virome.
Antibiotics saved millions of lives but their misuse or oversuse now raises serious concerns for health, notably with the further emergence of antimicrobial resistance. Each year, the World Health Organization (WHO) organizes the World AMR Awareness Week (WAAW) to increase awareness of this public health issue. Let’s take a look at this global threat that required urgent action:
Microbiota at the forefront of antibiotic resistance
A century on, and they’re back in the spotlight
In the 1920s, experiments to assess the therapeutic potential of phages gave promising results in patients with shigellosis, dysentery, and cholera. This (sidenote: Summers WC. The strange history of phage therapy. Bacteriophage. 2012 Apr 1;2(2):130-133. ) was then cast aside with the arrival of antibiotics in the 1940s. Although a few studies, unfortunately badly documented ones, continued in Soviet countries, phages were relegated to the second division. However, recent concerns over multidrug-resistant infections, and a new understanding of how antibiotics impact the balance of the intestinal microbiota, have prompted a renewed scientific interest in phage therapy. Each species of phage usually targets a single species of bacteria, which means these viruses can provide a “precision” solution where broad-spectrum antibiotics fall short. Nevertheless, despite its great promise, the health care authorities have yet to authorize any phage-based therapy (except in very exceptional cases).
What is the World AMR Awareness Week?
Each year, since 2015, the WHO organizes the World AMR Awareness Week (WAAW), which aims to increase awareness of global antimicrobial resistance. Held on 18-24 November, this campaign encourages the general public, healthcare professionals and decision-makers to use antimicrobials carefully, to prevent the further emergence of antimicrobial resistance.
Antibiotic resistance, dysbiosis, targeted therapy: multiple potential uses
(sidenote: Schooley RT, Biswas B, Gill JJ, et al. Development and Use of Personalized Bacteriophage-Based Therapeutic Cocktails To Treat a Patient with a Disseminated Resistant Acinetobacter baumannii Infection. Antimicrob Agents Chemother. 2017 Sep 22;61(10):e00954-17. ) attracted attention: a 68-year-old diabetic patient with pancreatitis complicated by a multidrug-resistant Acinetobacter baumannii infection regained full health in just five months thanks to phage therapy, after several failed attempts with antibiotics. Similar success stories have been reported with (sidenote: Jennes S, Merabishvili M, Soentjens P, et al. Use of bacteriophages in the treatment of colistin-only-sensitive Pseudomonas aeruginosa septicaemia in a patient with acute kidney injury-a case report. Crit Care. 2017 Jun 4;21(1):129. ) and (sidenote: Dedrick RM, Guerrero-Bustamante CA, Garlena RA, et al. Engineered bacteriophages for treatment of a patient with a disseminated drug-resistant Mycobacterium abscessus. Nat Med. 2019 May;25(5):730-733. ) , offering hope of a promising alternative for the treatment of multidrug-resistant bacterial infections. Phage therapy as a modulator of the intestinal microbiota is also of interest to scientists. A study in mice found that treatment with phages specific to Enterococcus faecalis, a bacterium associated with a poor prognosis in alcohol-related hepatitis, can improve the disease.
Other potential uses of phages are now being discussed, especially for precision medicine. These phages can transport potent cancer drugs and antibiotics to a precise area of the body, making it possible to increase the dose and reduce the toxicity of the treatment for adjacent tissues.
Seeking to overcome the challenges of clinical use
Research now needs to look at ways to overcome the many questions posed by clinical practice. Is phage therapy always safe? Can it replace antibiotic treatment? What is the best method of administration and the right dose? What is their long-term effect on the microbiota and health in general? According to the authors, randomized, double-blind, placebo-controlled clinical trials are needed to legitimize the role of phage therapy, an age-old practice that could help overcome several of the challenges facing medicine today.
Meet Professor Sørensen, 2022 Biocodex Microbiota Foundation International Grant Winner.
His team pioneered an ambitious study on the resistome of 700 children that will facilitate a breakthrough in the understanding of the evolution and dissemination of antimicrobial resistance in the early life human gut.






