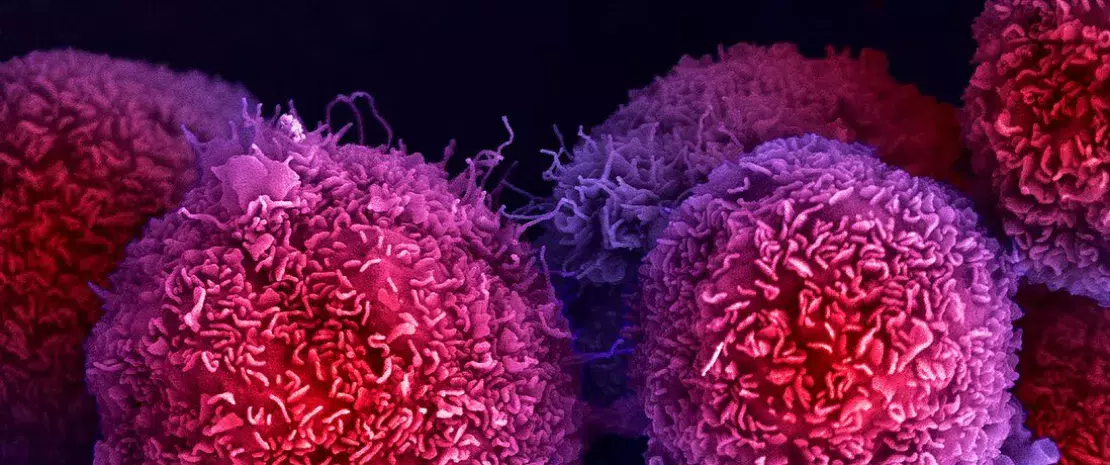
Pancreatic cancer: non-invasive early diagnosis thanks to the fecal microbiota?
Pancreatic cancer is one of the most difficult cancers to diagnose. Despite a low incidence rate, it has a particularly high mortality rate, due to late diagnosis and limited therapeutic options. Can the microbiota change this?
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Yes, according to the work of a German-Spanish team published in the journal Gut in 2022. Based on the observation that alterations in the oral, fecal, and pancreatic microbiota are associated with an increased risk of pancreatic ductal adenocarcinoma (PDAC), the researchers sought to assess the potential of the salivary and fecal microbiota as diagnostic tools for the disease. The only PDAC marker approved by the (sidenote: Food and Drug Administration US Federal Agency responsible for pharmacovigilance ) to date is carbohydrate antigen 19-9 (CA 19-9), which has limited sensitivity and specificity.
Diagnostic biomarkers identified via two cohorts
To evaluate the potential of the salivary and fecal microbiota as diagnostic biomarkers of PDAC, the researchers performed a metagenomic analysis (16S rRNA and shotgun sequencing) on fecal and saliva samples from two cohorts:
- The first cohort (prediction cohort) included 136 Spanish patients divided into three groups (57 PDAC patients who had not started treatment, 29 patients with chronic pancreatitis, 50 controls);
- The second cohort (validation cohort) included 76 German patients (32 PDAC patients, 32 controls).
Lastly, the specificity of the model was validated against 5,792 gut metagenomic profiles from 25 public databases.
Fecal microbiota: superior diagnostic performance
The fecal microbiota performed better (AUROC=0.84) than the salivary microbiota in accurately identifying patients with PDAC based on a set of 27 species, regardless of the disease phase (Spanish prediction cohort). Accuracy increased (AUROC=0.94) when fecal metagenomic analyses were combined with the serum marker CA 19-9. Both models were validated against the independent German cohort (AUROC=0.83) and against the gut metagenomic profiles of 5,792 patients across 18 countries suffering from various diseases (PDAC, obesity, diabetes, colorectal cancer, etc.): in both cases, PDAC-specific fecal metagenomic signatures were detected with accuracy. Lastly, several fecal PDAC marker species were detectable in pancreatic tumor and non-tumor tissue.
Towards new diagnostic methods?
The results of this study hold out hope for the early diagnosis of pancreatic cancer. They may lead to the development of a robust, non-invasive, low-cost, and effective method of detecting this type of cancer right from its early stages. Beyond diagnosis, the researchers suggest that these PDAC-specific bacteria may also open new prevention and therapeutic avenues for the disease.
Recommended by our community

"Very Good" -@TuCao50982078 (From Biocodex Microbiota Institute on X)







