New research finds that vaginal bacteria influences Group B Streptococcus colonization during pregnancy
New research reveals how shifts in vaginal bacteria during pregnancy influence the persistence of Group B Streptococcus, a hidden but dangerous pathogen. Scientists uncover microbial imbalances that could alter approaches to prenatal care and neonatal safety.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
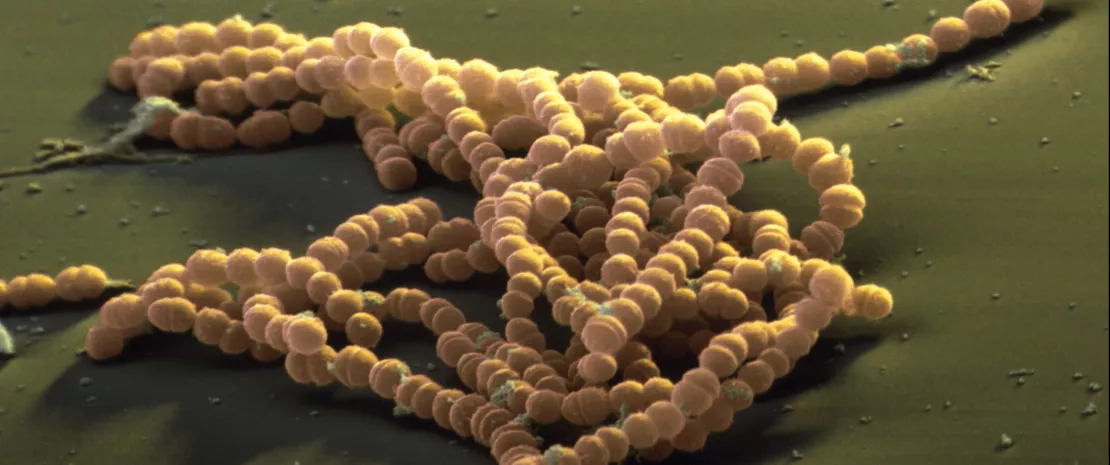
Author
(sidenote: Group B Streptococcus (GBS) A bacterium commonly found in the gastrointestinal and vaginal tract of adults, which can cause severe infections in newborns if transmitted during delivery. ) , a bacterium often residing silently in the human body, can become a significant threat during pregnancy. Its asymptomatic colonization in up to 40% of pregnant women can lead to neonatal complications like sepsis, pneumonia, and meningitis if transmitted during delivery. New research, led by Toby Maidment from the Queensland University of Technology, explored the interplay between (sidenote: Vaginal microbiota The community of microorganisms residing in the vaginal environment, primarily dominated by Lactobacillus species, crucial for maintaining reproductive health. ) and GBS colonization over time, providing groundbreaking insights into microbial dynamics. 1
Microbial shifts and persistent colonization
Using data from 93 pregnant women, they tracked microbial changes at 24 and 36 weeks of gestation, offering new clues about persistent and transient GBS colonization. One of the standout discoveries is the contrasting role of (sidenote: Lactobacillus crispatus A beneficial bacterium in the vaginal microbiota that produces lactic acid, maintaining a low pH to prevent pathogen colonization and infections. ) and (sidenote: Lactobacillus iners A less protective vaginal bacterium that produces only L-lactic acid, often associated with microbial imbalances and vulnerability to opportunistic infections ) . In women persistently colonized by GBS, L. crispatus, a key defender against pathogens, was significantly reduced. Instead, L. iners, a species less effective in maintaining vaginal acidity and microbial balance, was more abundant. This imbalance might create an environment that allows GBS to thrive.
Interestingly, transient GBS colonization (detected only at 24 weeks) was linked to more diverse microbial communities, dominated by species like Gardnerella vaginalis. By 36 weeks, this diversity declined, and L. crispatus along with L. iners became dominant, correlating with the resolution of GBS presence. This indicates a dynamic interaction where the vaginal microbiota may naturally shift toward a protective state, though not always effectively in persistent cases.
A closer look at GBS dynamics
Persistent GBS colonization often involved the same bacterial serotype across both time points, hinting at stable colonization mechanisms. Additionally, in persistently GBS-positive women, an average 11% reduction in GBS abundance was observed as pregnancy progressed, aligning with hormonal changes that increase Lactobacilli. However, despite this decline, the presence of L. iners continued to challenge the vaginal environment's resilience.
The study’s longitudinal design—tracking changes over time rather than a single snapshot—revealed that transient and persistent colonizations differ significantly in their microbial underpinnings. It also emphasizes the importance of addressing L. iners’ role in GBS colonization, as its presence may indicate a less protective vaginal environment compared to L. crispatus or other Lactobacillus species.
Before it’s too late!
This research presents a compelling case for personalized approaches to managing GBS in pregnancy. While L. crispatus emerges as a key player in vaginal health, L. iners seems less capable of offering protection against opportunistic pathogens. Understanding these dynamics could pave the way for interventions, such as probiotics targeted at increasing L. crispatus dominance or other strategies to bolster vaginal defenses.
Moving forward, microbial profiling may become a cornerstone of personalized obstetric strategies, potentially reducing the risks associated with GBS and improving neonatal outcomes.












