Key role of tumor bacteria in pancreatic cancer
The composition of pancreatic tumor microbiome, which is impacted by the gut microbiota, could modulate the patient’s immune response and the growth of adenocarcinoma. Could this discovery rekindle the interest in fecal transplants?
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
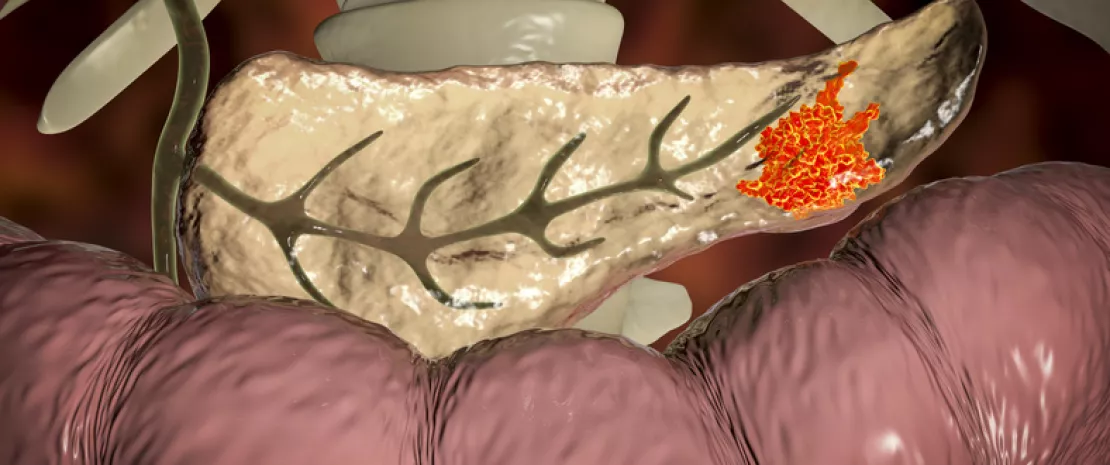
Pancreatic ductal adenocarcinoma (PDAC) is a dreaded cancer. As it is usually detected late, its prognosis is grim, with a 5-year overall survival rate of 9%. The tumor microbiota seems to play a role in this survival rate, based on the numerous results published in Cell by 31 researchers–mainly Americans.
More diversity = longer survival
To understand the impact of tumor microbiota and immune system on the long-term survival rate, these researchers analyzed the composition of the microbiota of resected tumors in 68 patients with PDAC divided into two groups: 36 patients who survived more than 5 years (mean: 10.1 years) and 32 patients who died less than 5 years after the procedure (mean: 1.6 years). Their results put forward a larger diversity of bacterial species present in the tumor microbiota of patients who survived more than 5 years. These results were confirmed by researchers in a second cohort.
Immune modulation
Moreover, the authors highlighted that each one of the two groups of patients displayed a specific intratumoral microbiota signature: presence and abundance of 3 bacterial genera (Pseudoxanthomonas, Streptomyces, Saccharopolyspora) and of Bacillus clausii are able to predict the survival in 97.51 to 99.17% of cases (according to the cohort). Additional immunohistological analyses suggest that the composition of the tumor microbiota could have an impact on cancer development by modulating the anti-tumor immune response through the recruitment and activation of CD8 T cells.
From the intestines to the tumor
In parallel, the analysis of stools, resected tumor tissues and adjacent non-cancerous tissues of three patients showed that the gut microbiota represents about 25% of the tumor microbiota, while it is absent from adjacent tissues: the tumor microbiota could thus be colonized by the gut microbiota. Finally, fecal microbiota transplants (FMT) from three types of patients (long-, short-term survival or control) were carried out in mice. These works confirmed the ability of the gut microbiota to colonize pancreatic tumors. They also suggested its ability to modify the bacterial composition of the tumor and, in turn, to modulate the immune function, thus affecting cancer progression and patient survival. Besides the possibility of formulating a prognosis based on the tumor microbiota, FMT results give us hope that one day we will be able to manipulate this microbiota to improve life expectancy of patients with PDAC, for whom very few therapeutic options are currently available.






