Influence of vaginal intercourse on male urogenital microbiota
The male urethra, which has been little described until now, is also thought to harbor microbiota. Vaginal intercourse could reshape its composition, making it a reservoir for the bacteria responsible for vaginosis in women.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
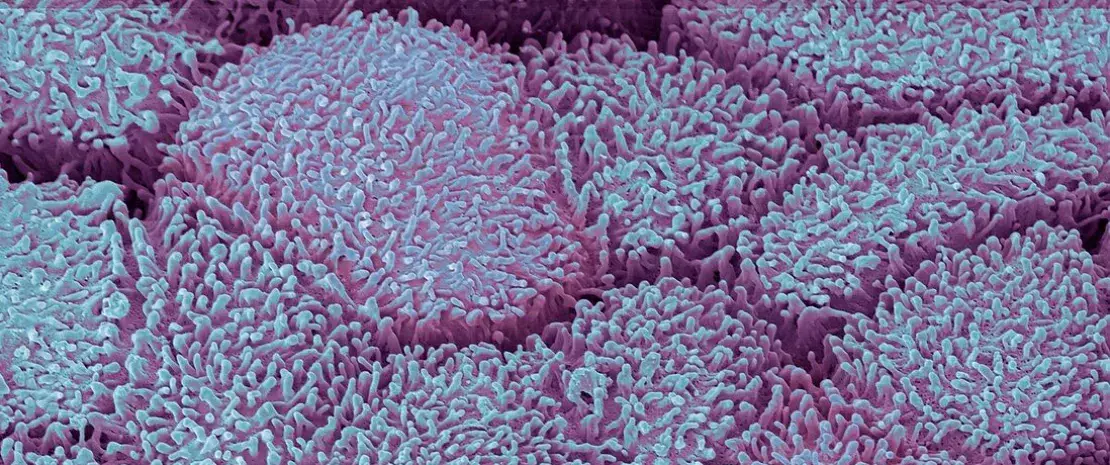
Little is known about male urethral microbiota, since sampling is painful and often reserved for men with sexually transmitted infections (STIs). However, there is increasing evidence to suggest that microorganisms colonize this mucosa, even in healthy individuals. An American study including 110 men with no urethral symptoms, infections or inflammation has finally uncovered them.
A “core” microbiota...
Most of the individuals were heterosexual. A swab was inserted 2 cm into each man’s urethra to analyze the microbiota (shotgun sequencing). In total, 117 different species of bacteria were detected. Most of the samples contained lactic acid bacteria (e.g., Streptococcus mitis) and corynebacteria, which could represent the “core” microbiota responsible for the health of the urethra. But that’s not all. Scientists have also identified bacteria in some men that are associated with bacterial vaginosis in women, in particular Gardnerella vaginalis. As a consequence, the male genital tract could be colonized by bacteria that are potentially pathogenic for women, even though on the whole its microbiota differs greatly from that of the vagina.
10% of the microbiota present in the male urethra is influenced by sexual intercourse, in particular vaginal penetration.
And two types of urethral microbiota
Two types of urethral microbiota (or urethrotypes, UT) were identified: type 1 microbiota (UT1) which is less abundant and diversified, mainly dominated by S. mitis, and type 2 microbiota (UT2) which is more abundant and diversified, dominated by G. vaginalis and composed of nine bacteria associated with vaginal disorders (bacterial vaginosis, vaginitis, etc.) and capable of forming biofilms with G. vaginalis. Given the bacteria’s degree of affinity for oxygen, researchers believe that these two microbiomes are located in different niches: UT1 is located close to the urinary meatus and UT2 slightly deeper.
In addition, UT2 is associated with vaginal intercourse and certain bacteria related to bacterial vaginosis are still detectable 60 days after sexual intercourse and, to a lesser extent, after a year or even over a lifetime. Vaginal intercourse in the last two months alone explains 4.26% of the variance in the composition of male urethral microbiota. And sexual practices as a whole (oral, vaginal, anal) account for around 10% of this variance.
Finally, no other variable, whether anal or oral intercourse, age, ethnicity or history of STI, was associated with either urethrotype.
Is bacterial vaginosis an STI?
The male urogenital microbiota could therefore be linked to sexual behavior and the male urethra could, in some men, harbor a wide range of agents that are potentially pathogenic for the female vaginal flora. Could they represent a reservoir for sexually transmitted microorganisms and risk contaminating women during unprotected sex? If so, shouldn't bacterial vaginosis be considered an STI? Currently it is not considered as such but this hypothesis (which is not new) will be explored in further research involving couples this time.
Recommended by our community

"Yes. Experts who contribute to the Embedded/Chronic UTIs support group on FB say the same about what used to be known as ‘Interstitial’ Cystitis." - Hazel Bowden (From Biocodex Microbiota Institute on X)










