Gut microbiota involved in the pathogenesis of non-alcoholic fatty liver disease
Press review
By Pr. Markku Voutilainen
Turku University Faculty of Medicine; Turku University Hospital, Department of Gastroenterology, Turku, Finland
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
About this article
Author
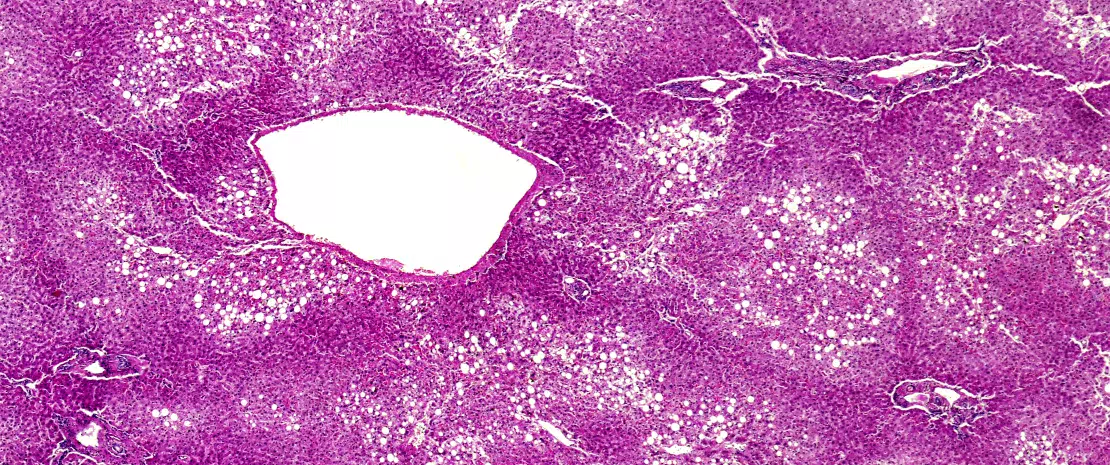
Non-alcoholic fatty liver disease (NAFLD) is the most common liver disease in western countries and affects 25-30% of the general population. NAFLD is classified into simple fatty liver disease with no or minimal inflammation, and steatohepatitis (NASH), which is characterized by steatosis, inflammation and fibrosis. NASH may lead to cirrhosis, which is a risk factor for hepatocellular carcinoma (HCC). NAFLD is the hepatic manifestation of metabolic syndrome.
Puri and Sanyal reviewed the role of the intestinal microbiome in NAFLD.[5] Increased adipose tissue mass with activation of the innate immune system leads to insulin resistance. Altered gut microbiota and increased intestinal permeability cause immune activation. Microbiome may also affect extra-intestinal organs by translocation, gut-derived neurohumoral signalling, and altering the nutritional substances absorbed from the intestine.
Chen and co-workers examined gut microbiota in the bile acid metabolism.[6] Microbiota produces enzymes that in the intestines convert primary bile acids (synthesised and conjugated in the liver) into secondary bile acids. Dysbiosis may lead to decreased synthesis of secondary bile acids, which in turn diminishes the activation of nuclear receptors such as farnesoid X receptor (FXR), pregnane X receptor, Takeda G-protein-coupled bile acid protein 5 (TGR5) and vitamin D receptor. These receptors play important roles in energy regulation and their dysfunction may play a role in the pathogenesis of NAFLD. Dysbiosis leads to increased bile acid deconjugation and is associated with disturbed lipid and cholesterol metabolism, weight increase and disturbed signalling.[6] Gut microbiota metabolises bile acids, conversely, bile acids are needed to maintain normal gut microbiota.
The gut microbiota is changed in NAFLD, but there is no uniform pattern.[6] Bacteria converting primary bile acids (C. leptum for example) are decreased in the faeces of NAFLD patients. Decreased FXR increases the synthesis of primary bile acids, gluconeogenesis, triglycerides and very-low-density lipoprotein synthesis. Thus decreased FXR as well as TGR5 may be involved in NAFLD pathogenesis. Modulation of gut microbiota could be an option for the treatment of NAFLD. Probiotics could adjust the whole bile acid pool instead of individual nuclear receptors.[6]
Variable definitions, histologic assessments and methods, as well as different bioinformatics approaches have been used. Thus it is difficult to draw generalisable conclusions of the microbiota changes in the pathogenesis of NAFLD.[5] The mechanisms that link microbiota changes to NAFLD pathogenesis are increased energy extraction in the gut and increased free fatty acid hepatic uptake, altered gut barrier function and endotoxemia with inflammation, altered bile acid and choline metabolism.
Loman and co-authors analysed the impact of pre- and probiotic treatment on NAFLD.[7] They identified 25 studies that fulfilled the PICOS* criteria: 9 assessed prebiotic, 11 probiotic and 7 symbiotic treatments. These therapies significantly reduced body mass index (BMI), hepatic transaminases and ν-glutamyltransferase, cholesterol and triglycerides levels. The effect of pro- and prebiotics were similar on BMI, liver enzymes and high-density cholesterol. The major weaknesses of the stu- dies were the lack of intestinal microbiota analysis, the heterogeneity of treatments, and their short duration. The present meta-analysis was, however, the first one to report simultaneous changes induced by microbiota treatment on weight, lipid metabolism and inflammation in NAFLD.







