Gut microbiota: defense against food allergies?
The risk of allergic reaction to b-lactoglobulin could be correlated to the composition of the gut microbiota. Increasing the levels of some species, especially Anaerostipes caccae, could protect against cow's milk protein allergy and become a new therapeutic approach.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Prevalence of food allergies steadily increases in Western countries. Among possible causes: gut dysbiosis related to new lifestyles (overuse of antibiotics, poor dietary habits, increased rate of cesarean deliveries...). This hypothesis was explored by an American team which focused on anaphylactic reactions in mice colonized by gut microorganisms extracted from children with or without b-lactoglobulin allergy.
Allergenic fecal transplant
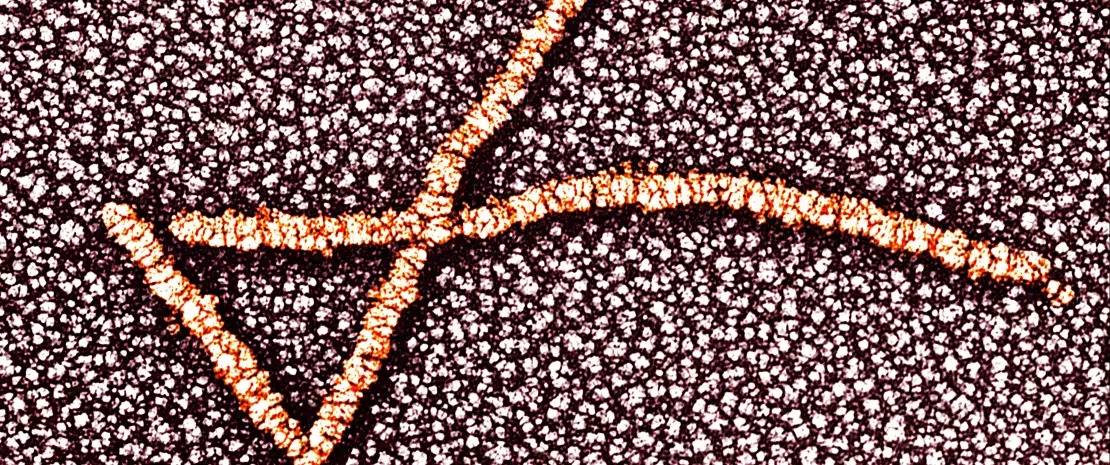
Fecal samples from 4 allergic newborns and 4 healthy newborns were administered to groups of axenic mice (germ-free mice), before exposing them to b-lactoglobulin. Result: “allergic” animals presented a sharp body temperature decrease and a significantly higher production of IgE and Ig1 anti-b-lactoglobulin antibodies and murine mast cell protease compared to “healthy” mice. However, mice who received a transplant from non-allergic children had no anaphylactic reaction and few temperature variations, thus suggesting the gut microbiota is involved in the mechanisms at play.
Protective vs. non-protective bacteria
Analyses carried out on the donors and on mice have shown notable variations of 58 (sidenote: Operational Taxonomic Unit groups of organisms usually not cultivated or not identified, classified on the basis of the similarity of the DNA sequencing of a given gene. Frequently used as an equivalent to the concept of species ) based on sensitivity to b-lactoglobulin allergens. 34 of them, from the Lachnospiraceae family, are qualified as “protective” (more abundant in healthy donors) and 24 as “non protective” (more abundant in allergic donors). Their relative abundance, expressed as a ratio, could be used to distinguish between allergic and non-allergic individuals.
Anaerostipes caccae: the ideal ileal bacteria?
Since tolerance to food allergens begins with absorption in small intestine, the team then characterized local bacterial populations and their potential action on the anaphylactic response. A beneficial species was thus identified in the ileum, where microorganisms of the small intestine are most abundant: Anaerostipes caccae (from the Lachnospiraceae family), whose increased content could be synonym of a better protection. This bacterium uses lactate and acetate and produces butyrate, three metabolites involved in the modulation of immune responses in the gastrointestinal tract. All these results highlight the role of commensal bacteria in food allergic reactions and open the way to the development of preventive and therapeutic strategies based on the modulation of the gut microbiota.






