From gut to bone: how microbiota affects fragility fracture risk
Will it soon be possible to reduce the risk of fragility fractures thanks to the gut microbiota? So suggests a study 1 linking this risk to the composition of the digestive flora
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
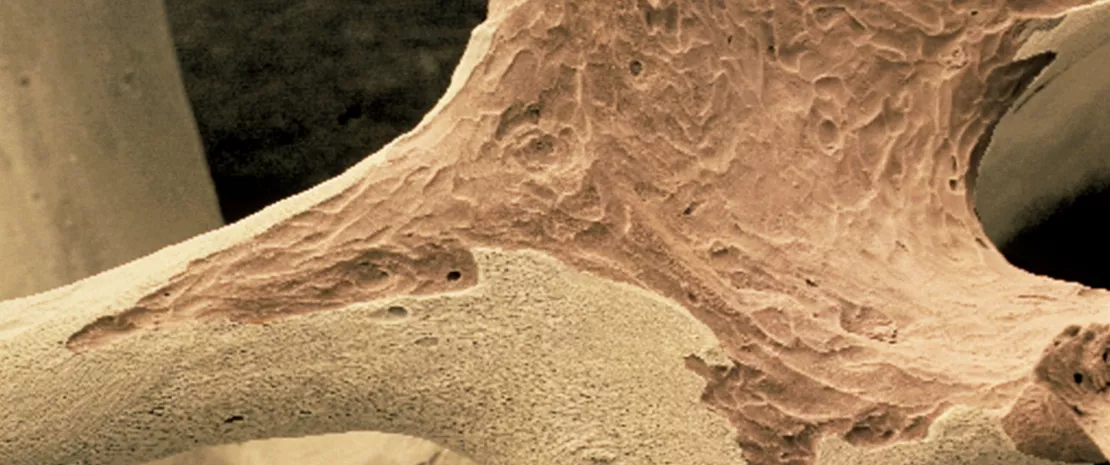
The increase in the number of bone fractures associated with an aging population represents a major public health concern, with one in two women and one in four men expected to suffer an osteoporotic fracture at some point. These fragility fractures most often result from a loss of bone mass that is difficult to prevent. Previous studies have shown a link between gut microbiota and bone mass in mice and humans. A new study has revealed that the gut microbiota also influences the risk of fragility fractures.
178 million
In 2019, there were 178 million new fractures globally, an increase of 33.4% since 1990, partly driven by population growth and ageing. 2
Microbiota composition, an indicator of fracture risk
The researchers used data from the FINRISK 2 cohort, which followed 7,043 Finnish subjects over 18 years. Metagenomic sequencing of the participants’ gut bacteria revealed that greater (sidenote: Alpha diversity Number of species coexisting in a given environment ) in the gut microbiota is associated with a reduced risk of fracture.
Of the ten most abundant phyla in the human microbiota, two appear to be particularly linked to bone fragility:
- Proteobacteria (including the pathogens Escherichia, Shigella, and Klebsiella), already implicated in various diseases (irritable bowel syndrome, etc.), are associated with an increased risk of fracture;
- On the contrary, Tenericutes (notably the genera Parabacteroides and Lachnoclostridium, and the three species Oscillibacter sp. ER4, Parabacteroides distasonis, and Dorea longicatena) appear to be associated with a reduced risk.
Could inflammation be the key?
As regards the mechanisms, a number of metabolic pathways have been implicated. Proteobacteria were associated with a reduced synthesis of branched-chain amino acids, which are known to be associated with bone health, and an increased production of pro-inflammatory microbial lipopolysaccharides. Tenericutes, on the other hand, are associated with the biosynthesis of anti-inflammatory (sidenote: Short chain fatty acids (SCFA) Short chain fatty acids (SCFA) are a source of energy (fuel) for an individual’s cells. They interact with the immune system and are involved in communication between the intestine and the brain. Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. ) (SCFA) such as butyrate. Proteobacteria and Tenericutes may therefore modulate inflammation, and with it bone resorption.
25.8 million Globally in 2019, fractures accounted for 25.8 million years lived with disability (YLDs), an increase of 65.3% in absolute YLDs since 1990. ³
+27% In the largest 5 countries of the European Union plus Sweden, the annual costs of fragility fractures are expected to increase by 27% by 2030. ³
Towards new fracture prevention strategies?
Although these results are promising, they are based on correlative analyses in a large but not very diverse population (Northern Europeans), and only on the predominant phyla of the gut microbiota (at the risk of overlooking the effect of rare phyla). Further research is therefore needed to establish a causal relationship between microbiota and fracture risk, and to understand the underlying mechanisms.
However, if these results are confirmed, treatments targeting microbiota imbalances could in future prevent osteoporosis and thus reduce the risk of fragility fracture.











