Could the gut microbiome be targeted to optimize Sars-CoV-2 vaccine efficacy?
Overview
By Dr. Genelle Healey
BC Children’s Hospital Research Institute University of British Columbia Vancouver, Canada
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections

About this article
Author
The primary goal of a successful SARS-CoV-2 vaccine, which is the main hope in controlling the Covid-19 pandemic, is to confer robust and long-lasting immunity for as many people administered the vaccine as possible. Despite several vaccines being deployed worldwide to manage the SARS-CoV-2 pandemic ongoing Covid-19 outbreaks demonstrate that the pandemic is far from over. Development of novelstrategies to help control the spread of the virus and/or enhance the efficacy of SARS-CoV-2 vaccines may prove useful in the fight against Covid-19.
SARS-COV-2 VACCINE EFFICACY
Vaccines are administered to challenge both the innate and adaptive immune systems. One common biomarker of lasting immunity and protection against SARSCoV- 2 are antibody responses. For reasons still poorly understood antibody responses to SARS-CoV-2 vaccination are highly variable between different people [1]. Based on results from clinical trials SARS-CoV-2 vaccine efficacy for approved vaccines ranges from around 60 to 92% against the original SARS-CoV-2 strains but vaccine- induced protection towards SARSCoV- 2 variants of concern (i.e., alpha, beta, delta, and gamma) appears to be lower [2]. Heterogenicity in vaccine responses between people, reduced vaccine efficacy with variants of concern and potential waning of vaccine efficacy over time all compromise the continued efforts to control the spread of SARS-CoV-2. Therefore, gaining a better understanding of the factors driving variations in SARS-CoV-2 vaccine efficacy in the short and long term is fundamentally important.
FACTORS THAT AFFECT VACCINE IMMUNOGENICITY
Given that everyone receives the same standardised vaccine dose, but immune responses vary widely, it is highly likely that factors other than vaccine type effect vaccine efficacy. Mounting evidence suggests that factors such as age, chronic disease, poor health behaviours, depression, and stress impact the immune system’s ability to respond to vaccines (Figure 1) [3-5]. These findings have been demonstrated across several vaccine types, so it is likely translatable to SARS-CoV-2 vaccines. Interestingly, most of the factors outlined above have also been shown to impact the composition and functional capacity of the gut microbiome. It is, therefore, plausible that gut microbiome dysbiosis driven by host factors could be implicated in the differing vaccine responses observed.
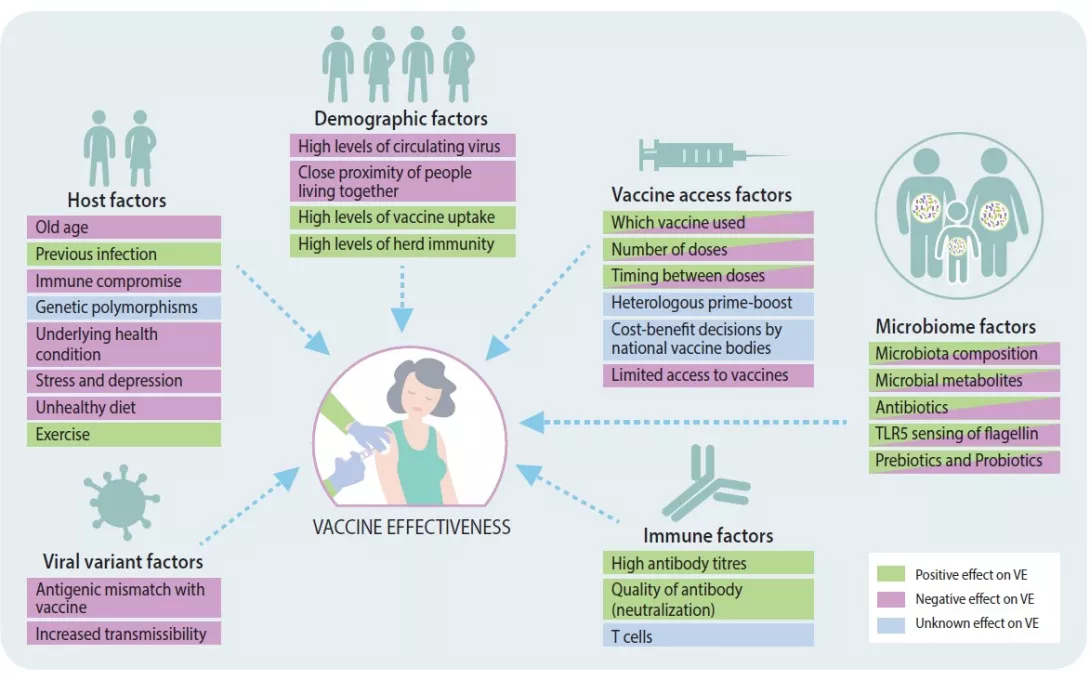
FIGURE 1
Factors influencing vaccine effectiveness.
Adapted from [14].
TARGETING THE GUT MICROBIOME TO ENHANCE VACCINE EFFICACY?
The gut microbiota is a collection of bacteria, fungi, viruses, and archaea that reside in the gastrointestinal tract and have co-evolved with their host over time. These microbes perform many important functions, one of which is regulating local and systemic immune responses. Interestingly, certain gut microbiota profiles (i.e., higher abundance of Actinobacteria, Clostridium cluster XI and Proteobacteria) have been associated with greater vaccine immunogenicity against viral infections such as HIV, influenza, and rotavirus [6-8]. A recent study reported that antibiotic-specific disruption of the gut microbiome (i.e., dysbiosis) led to impaired post influenza vaccine-induced antibody neutralization as well as lower concentrations of vaccine-induced antibody responses [9]. Another study using both antibiotic treatment and germ-free mice demonstrated that sensing of a bacterial motility component (flagellin) by a receptor found on immune cells (toll-like receptor 5 [TLR5]) was necessary in promoting a robust vaccine response [8]. This and other similar studies [10] provide evidence of the important role the gut microbiota plays in vaccine efficacy (Figure 1). However, to date no studies have investigated what impact the gut microbiota has on SARS-CoV-2 vaccine efficacy. Thus, future research which determines whether specific gut microbiota signatures impact SARS-CoV-2 vaccine efficacy are paramount. Additionally, microbiome-targeted therapies, i.e., prebiotics and probiotics [11], could be utilized as a vaccine adjuvant (an agent used to accelerate, enhance and/or prolong antibody specific immune responses) to enhance SARS-CoV-2 vaccine immunogenicity. Specifically, intranasal administration of lactic-acid bacteria (e.g., Bifidobacterium and Lactobacillus) has been shown to enhance resistance to viral infections and improve influenza vaccine efficacy [12, 13], therefore, oral delivery of live bacteria (probiotics) could boost vaccine specific immune responses if given alongside SARS-CoV-2 vaccines.
Conclusion
Irrespective of global vaccine deployment and targeted public health measures the Covid-19 pandemic continues to persist. Vaccines are the main hope in controlling SARSCoV- 2; however, heterogeneity in vaccine responses compromises the fight against Covid-19. Several gut microbiome factors have been implicated in altering vaccine immunogenicity. Therefore, utilisation of the gut microbiome as a vaccine adjuvant has the potential to improve SARSCoV- 2 vaccine effectiveness.
1 Amodio E, Capra G, Casuccio A, et al. Antibodies responses to SARS-CoV-2 in a large cohort of vaccinated subjects and seropositive patients. Vaccines 2021; 9(7): 714.
2 Gupta RK. Will SARS-CoV-2 variants of concern affect the promise of vaccines? Nat Rev Immunol 2021; 21(6): 340-1.
3 Collier DA, Ferreira IATM, Kotagiri P, et al. Age-related immune response heterogeneity to SARS-CoV-2 vaccine BNT162b2. Nature 2021; 596(7872): 417-22.
4 Grupper A, Rabinowich L, Schwartz D, et al. Reduced humoral response to mRNA SARSCoV-2 BNT162b2 vaccine in kidney transplant recipients without prior exposure to the virus. Am J Transplant 2021; 21: 2719-26.
5 Madison AA, Shrout MR, Renna ME, et al. Psychological and behavioural predictors of vaccine efficacy: Considerations for Covid-19. Perspect Psychol Sci 2021; 16(2): 191-203.
6 Harris VC, Armah G, Fuentes S et al. Significant correlation between the infant gut microbiome and rotavirus vaccine response in rural Ghana. J Infect Dis 2017; 215(1): 34-41.
7 Cram JA, Fiore-Gartland AJ, Srinivasan S, et al. Human gut microbiota is associated with HIV-reactive immunoglobulin at baseline and following HIV vaccination. PLoS One 2019; 14(12): e0225622.
8 Oh JZ, Ravindran R, Chassaing B, et al. TLR5-mediated sensing of gut microbiota is necessary for antibody responses to seasonal influenza vaccination. Immunity 2014; 41(3): 478-92.
9 Hagan T, Cortese M, Rouphael N, et al. Antibiotics-driven gut microbiome perturbation alters immunity to vaccines in humans. Cell 2019; 178(6): 1313-28.e13.
10 Harris VC, Haak BW, Handley SA, et al. Effect of antibiotic-mediated microbiome modulation on rotavirus vaccine immunogenicity: A human, randomized-control proof-of-concept trial. Cell Host Microbe 2018; 24(2): 197-207.e4.
11 Lei WT, Shih PC, Liu SJ, et al. Effect of probiotics and prebiotics on immune response to influenza vaccination in adults: a systematic review and meta-analysis of randomized controlled trials. Nutrients 2017; 9(11): 1175.
12 Belkina TV, Averina OV, Savenkova EV, Danilenko VN. Human intestinal microbiome and the immune system: The role of probiotics in shaping an immune system unsusceptible to Covid-19 infection. Bio Bull Rev 2021, 11(4): 329-43.
13 Taghinezhad S, Mohseni AH, Bermúdez-Humarán LG, et al. Probiotic-based vaccines may provide effective protection against Covid-19 acute respiratory disease. Vaccine 2021; 9(5): 466.
14 Tregoning JS, Flight KE, Higham SL, et al. Progress of the Covid-19 vaccine effort: viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat Rev Immunol 2021; 21(10): 626-36.







