Crohn’s disease: gut dysbiosis seems to precede flares
Crohn’s disease flare-ups could be preceded by a microbiota imbalance. Although patients do not have any early symptoms, some bacterial taxa levels could be reduced at the expense of others. Could this help us predict future flares?
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
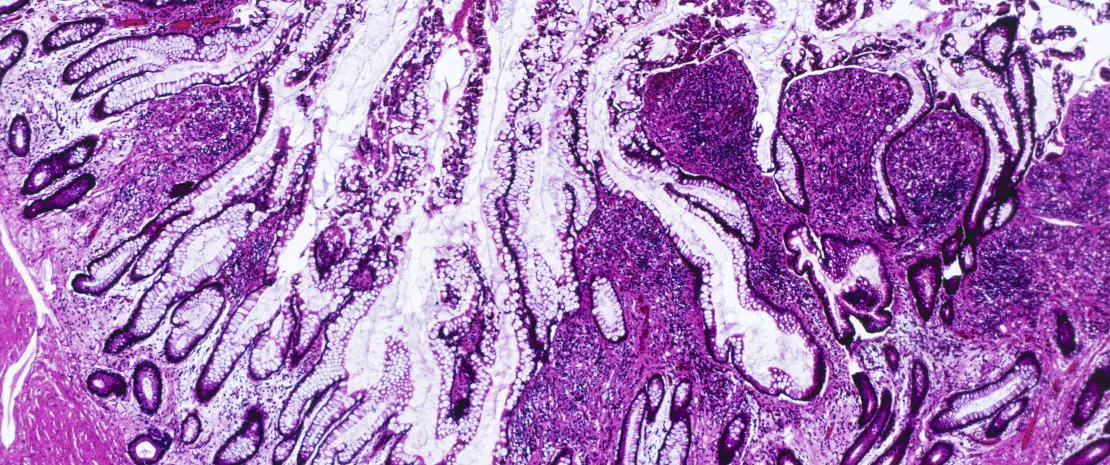
Crohn’s disease is an unpredictable and chronic disease, which progresses very variably from a patient to another. Although the causes of this inflammatory disease are not well known, it has been observed that patients’ gut microbiota seems to be less balanced than that of healthy subjects. But is it a cause of the disease, or a simple adaptation of the microbiota to an environment that has become inflammatory?
Two-year observational study
To get a clearer picture, a team of Israeli and American researchers monitored the microbiota of 45 patients in the remission phase of the disease. During this prospective observational study, the following tests were performed: analysis of gut microbiota, measurement of C-reactive protein (every 3 months) and fecal calprotectin levels, as well as endoscopic assessments (every 6 months). Results were compared to those of 17 patients in the inflammatory phase of the disease and to those of 22 control subjects. Objective: identifying whether flares are preceded by gut microbiota disruptions. To optimize the analytical process, the researchers used machine learning, a computer-based technology where analytical models are developed based on compiled data instead of prior programming.
Flares and microbiota instability
Results confirm that patients with Crohn’s disease have generally less abundant and more unbalanced microbiota (higher dysbiosis index) than healthy subjects. They mainly underline that in 27 out of the 45 patients who had a flare-up in the two-year follow-up period, they observed that this inflammatory phase was preceded by a significant decrease in the levels of some bacteria (Christensenellaceae and S24.7 families) and increase in others (Gemellaceae) compared to patients who remained in remission. Moreover, patients whose gut microbiota is more unstable in the resting phase of the disease are 11 times more likely to experiment an upcoming flare. Changes in the relative abundance of the three aforementioned taxa and global instability of the gut microbiota seem to precede flare‑ups, thus indicating that the gastrointestinal flora plays a role in flare pathogenesis. Despite the bias associated to machine learning (excessive individual variability compared to clinical factors), these results open the way to future tailored therapeutic options which could predict–and maybe one day prevent–upcoming flare-ups.






