Could the metabolome be used to better diagnose C. difficile infections?
Two large families of metabolites (the first are derived from leucine and the second from bile acids) could have the potential to discriminate between a C. difficile infection and an asymptomatic C. difficile colonization.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
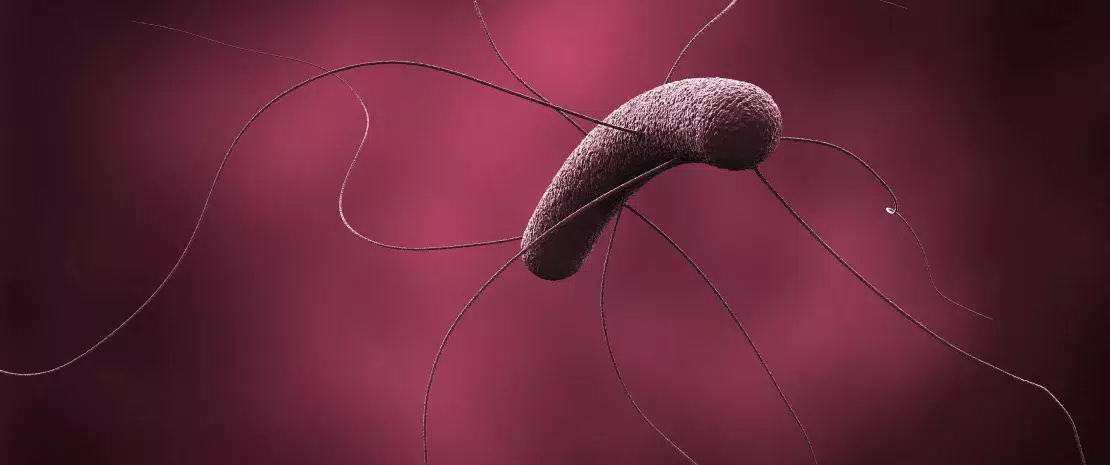
(sidenote: Clostridioides difficile formerly Clostridium difficile ) infection (CDI) affects about 450,000 people and causes 30,000 deaths per year in the United States. It is responsible for a substantial proportion of deaths attributable to antibiotic-resistant bacteria. CDI arises following the ingestion and adhesion of spores, which then germinate and turn into vegetative forms of the bacterium that colonize and secrete toxins responsible for a wide spectrum of symptoms ranging from diarrhea to life-threatening pseudomembranous colitis. But a carrier may also be completely asymptomatic and CDI may show its pathogenic potential only once antibiotics are taken.
Establishing a list of metabolites
C. difficile is considered as an opportunistic colonizer that might be eradicated by healthy intestinal microbiota. Several metabolic functions are believed to contribute to this eradication. To better understand the link between gut metabolites and CDI in humans, a research team studied the fecal metabolomic profiles of 186 hospitalized patients with symptoms of diarrhea: 62 patients with CDI (positive toxigenic culture and positive enzyme immunoassay), 62 patients with positive toxigenic culture but negative enzyme immunoassay, and 62 matched non-colonized controls (negative toxigenic culture and negative enzyme immunoassay). Fecal metabolites were characterized by gas chromatography.
Two metabolic signatures
Among the 2,463 metabolites detected in the stools, 43 can be used to discriminate between patients with CDI and non colonized controls. Many of them are derived from (sidenote: The Stickland fermentation pathway coupled redox reaction of two amino acids, one playing the role of hydrogen acceptor, the other of hydrogen donor. It occurs in many Clostridium species de Vladar HP. Amino acid fermentation at the origin of the genetic code. Biol Direct. 2012 Feb 10;7:6. ) , in which bacteria, such as C. difficile, use amino acids as substrates. The strongest association found was for a short chain fatty acid resulting from leucine fermentation, which was found in significantly larger quantities in patients with CDI. The team also identified a number of secondary bile acids significantly less abundant in patients with CDI, and derived from the dehydroxylation by gut bacteria of primary bile acids which are synthesized and conjugated by the host. It remains unclear whether these dehydroxylated bile acids are only biomarkers of CDI-negative patients, or if their formation protects them from CDI by inhibiting spore germination, for instance.
Towards a more precise diagnosis?
Eventually, these results could lead to the definition of a specific metabolomic profile for CDI and refine patient diagnosis, by reducing false positives related to inactive spore detection by toxigenic culture, and false negatives caused by the poor sensitivity of the enzyme immunoassay.






