Could the gut microbiota be a tuberculosis signature?
While tuberculosis-associated disruptions of the gut microbiota have already been described, a study went even further in the characterization of this dysbiosis and identified some species that signal this disease.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
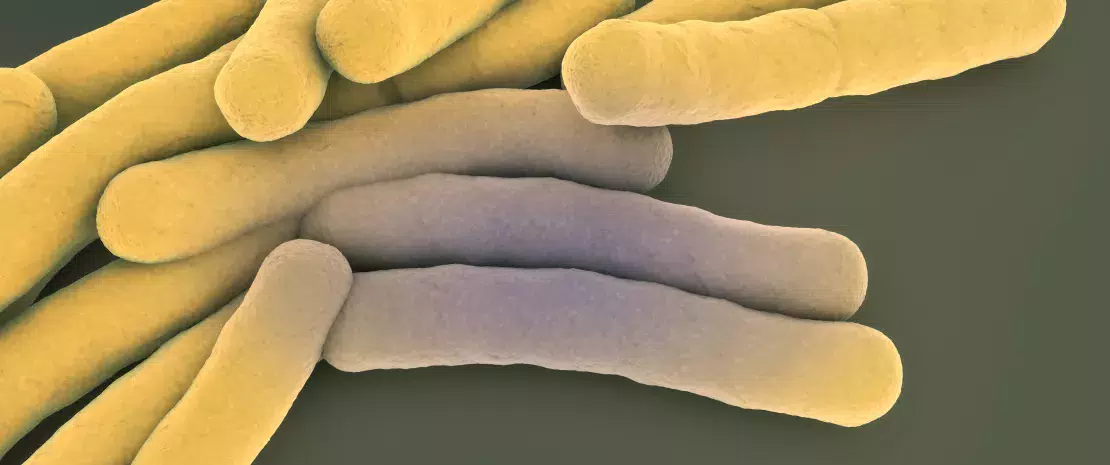
The ability of the gut microbiota to remotely communicate with organs such as the brain, liver or lungs has often been reported in the scientific literature, as well as associations between dysbiosis and some diseases. In this context, a Chinese team focused on the gut microbiota specificities of patients with tuberculosis (TB) caused by Mycobacterium tuberculosis.To describe them, the researchers compared the microbiota of 46 patients with TB to that of 31 control subjects, using (sidenote: Shotgun sequencing method is more accurate than 16S rARN. ) .
Less diversified gut microbiota
First finding: the microbiota of patients with TB showed significantly lower bacterial abundance and diversity (Shannon index). It was also characterized by a decreased or increased presence of some species compared to the control group. In total, 23 species were less abundant in the microbiota of patients with TB, while 2 were more abundant (unclassified Coprobacillus and Clostridum bolteae).
Decreased SCFA metabolism
Another notable finding: among the 23 decreased bacterial species in patients with TB, 9 produce short-chain fatty acids (SCFA), components which are largely involved in inflammatory and immune responses. In particular, five butyrate-producing species (Roseburia inulinivorans, R. hominis, R. intestinalis, Eubacterium rectale and Coprococcus comes), two lactate- and acetate-producing species (Bifidobacterium adolescentis and B. longum) and two acetate- and propionate- producing species (Ruminococcus obeum and Akkermansia muciniphila) were found in decreased amounts. In line with these changes in bacterial composition, SCFA fermentation was significantly lower in patients with TB.
Identifying tuberculosis patients based on their microbiota?
Finally, based on modeling studies, the researchers characterized 3 bacterial species (Haemophilus parainfluenzae, R. inulinivorans and R. hominis) whose presence could discriminate between healthy and tuberculosis patients. The healthy and diseased states could also be distinguished by some genetic variations (SNP, Single Nucleotide Polymorphism) in the B. vulgaris species. As for several disorders affecting different body systems (type 2 diabetes, autism, etc.), tuberculosis seems to be associated to a dysbiosis of the gut microbiota. However, it is not yet possible to determine whether it is a cause or a consequence of the disease, since mechanistic data currently available from animal studies are compatible with both hypotheses.






