The role of Fusobacterium in colorectal cancer
Commented article - Adult section
By Pr. Harry Sokol
Gastroenterology and Nutrition, Saint-Antoine Hospital, Paris, France
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
About this article
Author
Comments on an original article by Bullman et al. (Science 2017)
Colorectal cancers (CRCs) comprise a complex mixture of malignant cells, nontransformed cells, and microorganisms. Fusobacterium nucleatum is one of the most prevalent bacterial species in CRC tissues.
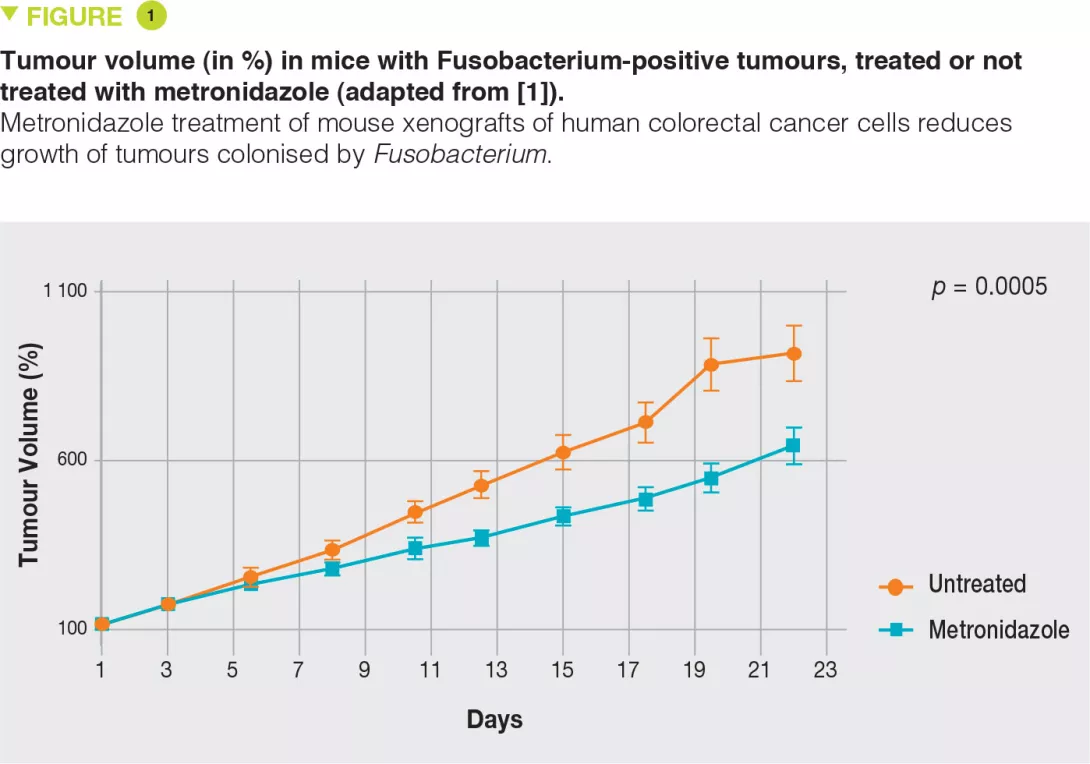
Here, the authors show that colonisation of human CRC with Fusobacterium and its associated microbiome (including the Bacteroides, Selenomonas and Prevotella species) is maintained in distal metastases, demonstrating microbiome stability between paired primary and metastatic tumours. In situ hybridisation analysis revealed that Fusobacterium is mainly associated with cancer cells in metastatic lesions. In mouse xenografts of human primary colorectal adenocarcinomas, Fusobacterium and its associated microbiome remains viable despite successive passages. Treatment of CRC xenografted mice with metronidazole, an antibiotic, reduces Fusobacterium load, cancer cell proliferation, and overall tumour growth.
These observations should prompt further investigation of antimicrobial interventions as a potential treatment for patients with Fusobacterium-associated CRC [1].
What is already known about this topic?
Cancer-associated microbiota is known to influence cancer development and progression, including CRC. The microbiota of CRC patients is dysbiotic, and several studies conducted without any preconceptions have revealed an enrichment in F. nucleatum in tumour tissues and adenomas compared to non-cancerous colonic tissues [2]. These findings have been confirmed in studies conducted worldwide based on several cohorts of CRC patients. High levels of F. nucleatum have been associated with less T-cell tumour infiltration (T-cell infiltration is, however, a factor of good prognosis) [3], advanced disease, and a lower rate of patient survival. In addition, patients with F. nucleatum- associated CRC often presented with a right colonic location of cancer, BRAF mutation, and microsatellite instability. Studies based on various experimental models have suggested a protumourigenic role of Fusobacterium, which potentiates tumour growth in mouse models of CRC, xenografts derived from CRC cell lines, and in vitro CRC cell lines. The suggested mechanisms range from increased adhesion and invasion of tumour cells to modulation of the host immune response or activation of the Toll-like receptor 4 pathway. However, some animal or cellular studies have shown no carcinogenic effects of Fusobacterium [4].
What are the main results of this study?
To explore the role of Fusobacterium and its associated microbiota in CRC, the authors analysed the microbiota of five independent cohorts of CRC patients. For frozen samples (11 cases), the culture-based detection of Fusobacterium was positive in more than 70% of cases, showing that the bacterium was alive within the tumour tissue. Furthermore, when metastatic tissue was available and of good quality, Fusobacterium was also detected using culture methods. The molecular method (qPCR) demonstrated greater sensitivity, with more than 80% and more than 60% positivity for primary and metastatic tissues, respectively. The Fusobacterium identified in metastatic tissues was the same as that identified in the primary lesion. In addition to Fusobacterium, other bacteria with the same profile were identified, such as Bacteroides fragilis or Bacteroides thetaiotaomicron, however, unlike Fusobacterium, the strains identified in metastases were different from those identified in the primary lesion. In a cohort of 77 patients, the authors observed that there was no link between positive Fusobacterium culture and tumour recurrence. To determine whether the presence of Fusobacterium plays a role in carcinogenesis or is only passively involved in the oncogenic process, the authors used several systems, including human tumour cell xenografts in immunodeficient mice. They observed that Fusobacterium-positive tumours were easily implanted in mice while this was not the case for Fusobacterium-negative tumours. Finally, treatment with metronidazole, a highly active antibiotic targeting Fusobacterium, significantly reduced tumour growth (Figure 1).
Key points
-
Fusobacterium is present in a viable form in primary and metastatic tissues in most CRC patients.
-
When present, Fusobacterium promotes tumour growth.
-
In murine models, antibiotic treatment targeting Fusobacterium significantly reduces the growth of Fusobacterium positive tumours.
What are the practical consequences?
The treatment of metastatic CRC remains a major clinical issue. This study shows that some bacteria of the microbiota, especially those belonging to the Fusobacterium genus, continue to be viable in both the primary tumour and metastatic tissues in most patients, and play a role in CRC progression. The use of antimicrobial treatments targeting these bacteria is therefore a strategy to be considered, while trying to be as specific as possible, because other bacteria may play a protective role or be involved in the response to conventional anticancer therapies and immunotherapies [5].
Conclusion
Based on several independant cohorts, this study shows that Fusobacterium is present in a viable form in primary and metastatic tissues in the majority of CRC patients, and is suggested to play a role in promoting tumour progression. These observations should prompt further investigation of antimicrobial interventions as a potential treatment for patients with Fusobacterium-associated CRC.







