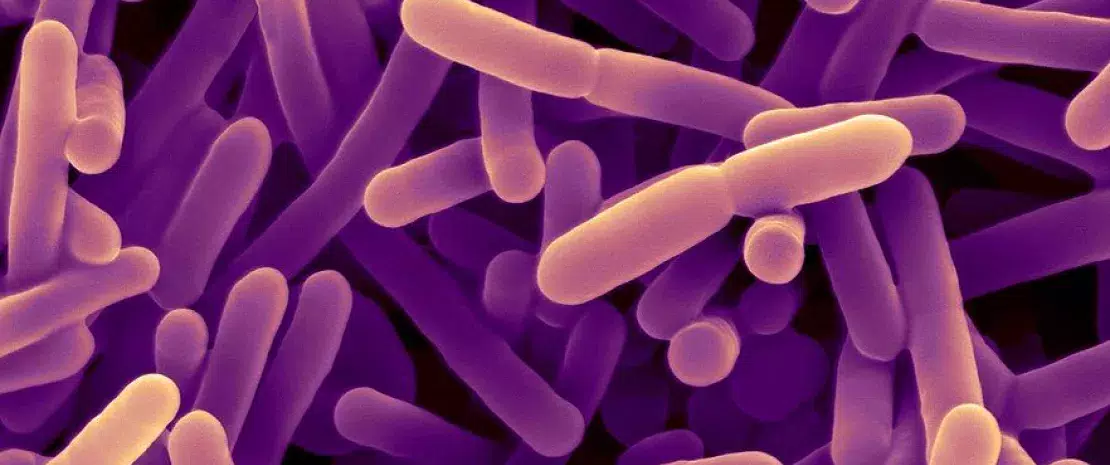
The role of Bifidobacteria in irritable bowel syndrome (IBS)
A low-FODMAP diet may reduce gut bifidobacteria in patients suffering from irritable bowel syndrome (IBS). The bacterial species Bifidobacterium adolescentis may be involved in the increase of gut barrier permeability.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction (DGBI), which are also known as functional bowel disorders (FBD). It causes chronic abdominal pain and transit disorders leading to a significant deterioration in quality of life. 1 Many patients associate IBS with their diet, thus justifying dietary approaches, sometimes empirical, in an attempt to reduce symptoms. A systematic review 2 examined the effect of one such approach, a diet low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs).
Effect limited to bifidobacteria
This meta-analysis included 9 randomized controlled trials involving a total of 403 patients. Apart from a clear reduction in the abundance of bifidobacteria, this dietary approach had inconsistent or minimal effects on microbiota composition and metabolism. It had no clear impact on microbiota diversity, which the authors consider reassuring, since higher diversity is considered a hallmark of gastrointestinal health, while lower diversity is associated with disease states.
The diet did not have any clear effect on bacterial load either, even though it supposedly works by reducing the availability of fermentable carbohydrates in the colon, limiting the major substrates available for bacterial proliferation.
Fecal concentrations of SCFAs were also unaffected. However, since most SCFAs produced are absorbed in the colon, the fecal concentration may not be reflective of the luminal concentration.
The only real effect observed by several trials
The only real effect observed in several trials was a decrease in the abundance of bifidobacteria following the removal of fermentable carbohydrates from the diet. This finding suggests that FODMAPs are a major substrate for bifidobacteria, which are known to metabolize (sidenote: Fructanes Polymers consisting of a glucose molecule linked to several fructose molecules. ) .
A reversible anti-bifidogenic effect
The anti-bifidogenic effect of the low-FODMAP diet is a cause for concern. Bifidobacteria have immunomodulatory and anticancer properties (animal studies) and a lower abundance of bifidobacteria has been associated with a greater severity of IBS symptoms in humans. However, according to the authors, this concern should be put into perspective, at least for short-term diets (3 to 4 weeks): a recent trial showed a restoration of bifidobacteria abundance upon completion of the diet, while bifidobacteria supplementation was sufficient to reduce the anti-bifidogenic effect.
Thus, three to four weeks on a low-FODMAP diet induces a dysbiosis limited to bifidobacteria, without implications for the composition and functioning of the gut microbiota. According to the authors, this alleviates concerns about the safety for the colonic microbiota of a short-term low-FODMAP diet. However, the effects of long-term interventions are not yet known.
Your IBS Diagnosis Check List
Could the answer lie in the tight junctions?
A second publication 3 has contributed further to this issue. To establish potential causal relations between specific microbial taxa and their functional impact on host tissues, an Israeli team infused mouse digestive tract cultures into solutions containing microbiota samples collected from IBS patients who had successfully followed a low-FODMAP diet for six weeks. In patients who benefited from this diet (3 out of 10), bifidobacteria, and particularly Bifidobacterium adolescentis, were less present in the gut microbiota as the diet progressed (at three weeks and then at six weeks). More importantly, ex vivo cultures show that the post-diet microbiota (lower in bifidobacteria) modulates the intestinal expression of genes involved in inflammatory and neuromuscular processes and in the tight junctions between cells of the digestive wall. In addition, the team identified B. adolescentis as a potent disruptor of intestinal epithelium tight junction integrity and of gut barrier functions. In low-FODMAP diets, the reduced presence of B. adolescentis may result from lower fructose availability. This finding therefore leads us to wonder about the reverse situation, i.e. Western diets rich in fructose that are associated with gut barrier deterioration, low-grade inflammation, and endotoxemia: could the observed pathological consequences of excess fructose consumption be mediated, at least in part, by dysbiotic B. adolescentis overgrowth?
This study is a first step in identifying the mechanisms at work in the microbiota’s mediation of the beneficial effects of a low-FODMAP diet. It also supports the feasibility of microbiota-based therapies for these patients, whether through fecal transplantation or probiotics.
2. So D, Loughman A, Staudacher HM. Effects of a low FODMAP diet on the colonic microbiome in irritable bowel syndrome: a systematic review with meta-analysis. Am J Clin Nutr. 2022 Oct 6;116(4):943-952.
3. Bootz-Maoz H, Pearl A, Melzer E et al. Diet-induced modifications to human microbiome reshape colonic homeostasis in irritable bowel syndrome. Cell Rep. 2022 Nov 15;41(7):111657.







