Microbiota and cystic fibrosis
Press review
By Pr. Ener Cagri Dinleyici
Professor in Pediatrics, Eskisehir Osmangazi University Faculty of Medicine; Department of Pediatrics, Eskisehir, Turkey
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
About this article
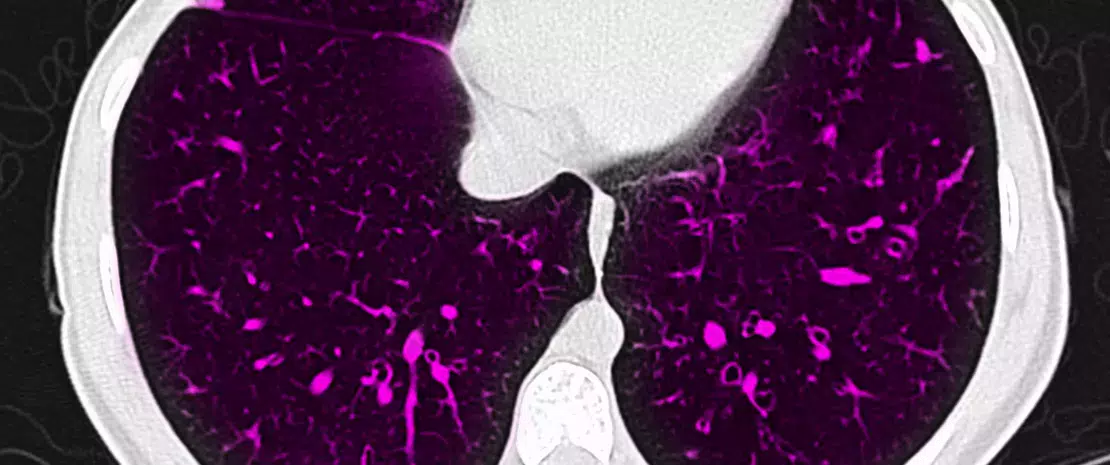
Author
Cystic fibrosis (CF) is a progressive, genetic disease that causes persistent lower respiratory infections and is related to different systemic symptoms and signs. More than 70,000 people live with CF worldwide [1].
The types and severity of symptoms can differ widely from person to person and are mainly related to the age of the patient as well as age at diagnosis. Children and adolescents with CF have a wide range of symptoms and signs including gastrointestinal manifestations. Recent studies have shown that dysbiosis is a feature of CF, leading to reports focusing on the relationship between the composition of the airway microbiota and clinical features and pulmonary function in patients with CF [2].
Dysbiosis-associated CF may be related to the natural course of the disease (including gastrointestinal involvement or respiratory microbiota alterations). However, patients require multiple courses of antibiotic treatment and these antibiotics may change the composition of the microbiota.
Studies have shown that patients with CF typically have decreased amounts of Bifidobacterium spp., Bacteroides-Prevotella group, Clostridium cluster XIVa, Faecalibacterium prausnitzii and Eubacterium rectale, whereas Enterobacteriaceae and Clostridia are increased. De Freitas and colleagues published a recent study in PLOS One, aimed at evaluating the effect of CF and antibiotic therapy on the intestinal microbiota composition in 19 children and adolescents with CF relative to 17 age and sex-matched controls [3]. The level of fecal calprotectin (an intestinal inflammation marker) was higher in the CF group (irrespective of antibiotic treatment) compared to the healthy controls. The authors showed that Bacteroides, Firmicutes, Eubacterium rectale and Faecalibacterium prausnitzii were significantly decreased, whereas Clostridium difficile, Escherichia coli and Pseudomonas aeruginosa were significantly increased in the CF group, relative to the healthy controls. The main differences in microbiota composition between patients with CF and controls, irrespective of antibiotic treatment, were noted for Eubacterium rectale, Bifidobacterium, Escherichia coli, Firmicutes, Pseudomonas aeruginosa and Clostridium difficile. The results of this study therefore demonstrate that the intestinal microbiota composition in CF patients is different from that of healthy controls and that the frequent use of antibiotics has no additional effects on these alterations.






