Gut microbiota: a new player in prostate cancer therapies?
Researchers have brought to light how the gut microbiota interacts with an oral drug used to treat prostate cancer, thus indicating that certain bacteria play a significant role in response to treatment.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
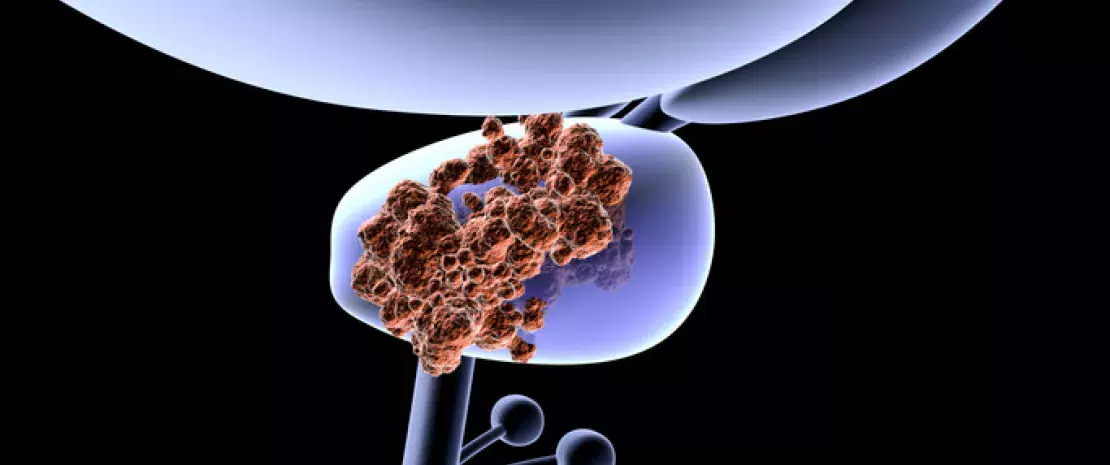
Standard therapies designed to deprive the body of androgens, which are responsible for the growth of prostate cancer, are not always effective. In such cases, abiraterone acetate (AA) is used, and unlike other treatments, it is taken orally. Since AA is poorly absorbed, a significant portion of it is excreted in the stool and interacts with the gut microbiota. Several studies have highlighted the role of the gut microbiota in the development and progression of certain cancers, and in the effectiveness of treatments. However, there are still few data on the gut microbiota’s role in prostate cancer. The researchers therefore sought to show how AA (highly effective in hormone-refractory prostate cancer) affects the gut microbiota, and to assess whether the latter can influence responses to treatment.
Androgen deprivation remodels the gut microbiota
To this end, they used 16S rRNA sequencing to examine the gut microbiota composition of 68 prostate cancer patients divided in three groups:
- treatment-naive patients (n=33) ;
- patients receiving standard therapy (n=21) ;
- patients receiving standard therapy + AA (n=14)
Compared with the control group, standard therapy alone or standard therapy combined with AA led to a significant reduction in Corynebacterium, pro-inflammatory bacteria that metabolize androgens such as testosterone. AA intake led to a significant enrichment of Akkermansia muciniphila and increased production of vitamin K2, known for its anti-tumor properties.
A. muciniphila plays a key role in response to treatment
These results were confirmed in a simulated gut model, which excluded the possibility of immune involvement. Further investigations revealed that AA is metabolized by gut bacteria. Compounds derived from this degradation selectively impact the gut microbiota, characterized by the growth of A. muciniphila. This bacterial species known for its health benefits and anti-inflammatory properties is thought by the authors to play a key role in treatment response. Previous work had brought to light its beneficial role in responses to certain immunotherapies. This study highlights the gut microbiota’s key role in responses to an oral anti-cancer treatment, via mechanisms yet to be elucidated. Exploring drug-microbiota interactions could improve treatment outcomes for numerous diseases.






