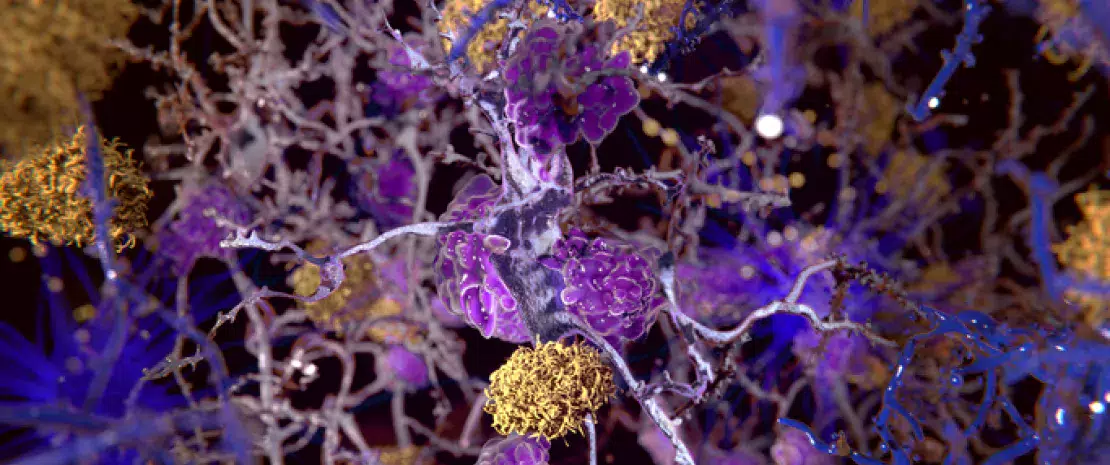
Alzheimer’s: how gut dysbiosis influences amyloid pathology
A recent study clarifies the gut microbiota’s role in the amyloid pathology associated with Alzheimer’s disease. This role involves bacterial compounds capable of reaching the brain following a systemic inflammatory reaction.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
The presence of a gut dysbiosis in patients suffering from Alzheimer’s disease has already been proven. So too has the microbiota’s involvement in the cerebral accumulation of amyloid beta proteins associated with the disease. This new study aimed to investigate the signaling pathways through which patients’ gut microbiota contributes to this amyloid pathology.
In search of correlations
The study involved 89 individuals aged between 50 and 85 with cognitive performance ranging from normal to cognitive impairment with memory loss (whether or not associated with the disease). Amyloid deposits were measured by PET-scan and quantified in the various areas of the brain, while blood levels of molecules produced by the gut microbiota (lipopolysaccharides–LPS–and short-chain fatty acids–acetate, propionate, valerate, butyrate), pro- and anti-inflammatory biomarkers (including interleukins–ILs) and biomarkers of endothelial dysfunction (cell adhesion molecules–CAMs) were also measured.
Bacterial mediators implicated
Regardless of the brain area, amyloid deposition was positively correlated with blood levels of LPS, acetate, valerate, certain pro-inflammatory cytokines (e.g. IL1b, IL6) and many CAMs (e.g. P-selectin, PECAM-1), but negatively correlated with butyrate and IL10 (anti-inflammatory) levels. Lastly, some biomarkers of endothelial dysfunction were positively correlated with acetate, valerate, IL1b and IL4 levels, but again negatively correlated with levels of butyrate and IL10. The authors interpreted these correlations as evidence of a direct and indirect association between blood parameters linked to gut dysbiosis and amyloid pathology.
Inflammation, barrier function and Alzheimer’s
Therefore, the reduction in butyrate levels associated with an increase in the levels of acetate, valerate and LPS may compromise the integrity of the gut barrier, cause and maintain low-level systemic inflammation, and alter the blood-brain barrier, ultimately allowing pro-inflammatory compounds facilitating the pathological cascade of Alzheimer’s disease to enter the central nervous system. While highlighting that no causal link could be established from their data, the authors emphasize that the strength of the associations found supports this pathophysiological hypothesis. Lastly, it may be possible to develop prevention strategies for Alzheimer’s based on enriching the microbiota with beneficial bacteria or metabolites, once the microbial signature associated with the disease has been clarified.






