Focus on diabetes
Diabetes3 could become the 7th highest cause of death in the world by 2030 according to the WHO, bringing its share of strokes, amputations, blindness and dialysis. A scourge which could be partly combatted by a healthier lifestyle… and perhaps by working on our intestinal flora, provided that we can unravel its multiple actions on our metabolism.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information
Sections

About this article
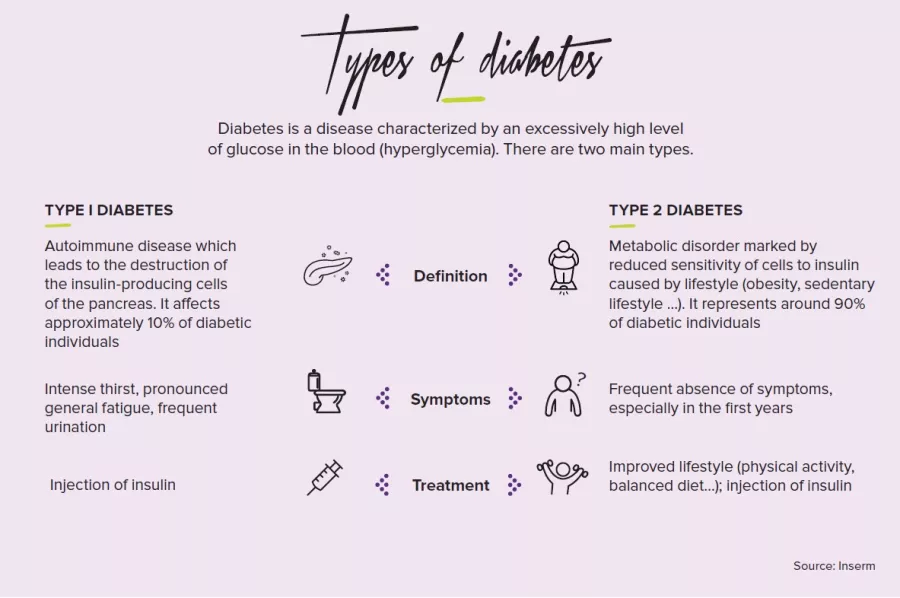
It has been known for a long time that diabetes is associated with sugars. However, it is also associated with intestinal bacteria which enable us to digest slow sugars (starch and other dietary fibers) by breaking them down into simple sugars which ferment into short chain fatty acids (SCFA) and, inevitably, gas. However, individuals with type 2 diabetes are thought to have a microbiota less rich in bacteria that produce these famous SCFA. Other bacteria have less beneficial effects: they cause chronic inflammation of the liver through accumulation of fats (the famous “NASH”, or non-alcoholic steatohepatitis). Some also release toxic substances when they die, whose presence in the blood is associated with an increased risk of diabetes. Furthermore, as 90 to 95 % of diabetics are also obese, they suffer from the chronic inflammation found in obesity, partly generated via the intestinal microbiota.
Bacteria which tilt the balance
In type I diabetes, where the immune system turns against the pancreatic cells responsible for insulin production (beta cells), the composition of the microbiota changes: a flora less rich in Proteobacteria and overabundance of Firmicutes relative to Bacteroidetes are thought to be some of the risk factors. Conversely, some bacteria (lactobacilli, bifidobacteria, bacteria that produce butyric acid) could provide protection against autoimmunity, a deregulation which forces us to fight against our own immune defenses. Finally, there are also other members of the microbiota– i.e. viruses–such as Coxsackie viruses4 that are capable of infecting the insulin-producing cells of the pancreas.
On the track of elucidating treatment mechanisms
To complicate matters, bacteria are also thought to influence the actions of metformin. This drug used in first line treatment of type 2 diabetes is thought to reduce the inflammation caused by toxic bacterial substances while reducing the absorption of fats… via the intestinal flora. This might shed light on its mode of action which is still unclear, but could also bias the results of studies conducted in these patients. These are all mechanisms among many others which link diabetes and the intestinal microbiota, whose vast and complex field of action we are barely beginning to discern
4 Exclusively human viruses belonging to the enterovirus family (which reproduce in the intestines)