Gut microbiota widely implicated in functional dyspepsia
Functional dyspepsia is a very common reason why people go to the doctor and is often treated with antibiotics. A recent review has highlighted the promise of a less aggressive solution: modulation of the microbiota.
Sources
This article is based on scientific information
About this article
A heavy feeling in the stomach after eating, feeling full too early in a meal, epigastric burning – just some of the disabling symptoms of functional dyspepsia (FD), a common disorder of the gastrointestinal tract that gives rise to numerous medical complaints. The prevalence of FD is high, estimated at 7.2% worldwide, with women, smokers, and patients taking non-steroidal anti-inflammatory drugs at particular risk. The gut microbiota may be involved.
250-400 m2 the human digestive system is the largest exchange surface in the body.
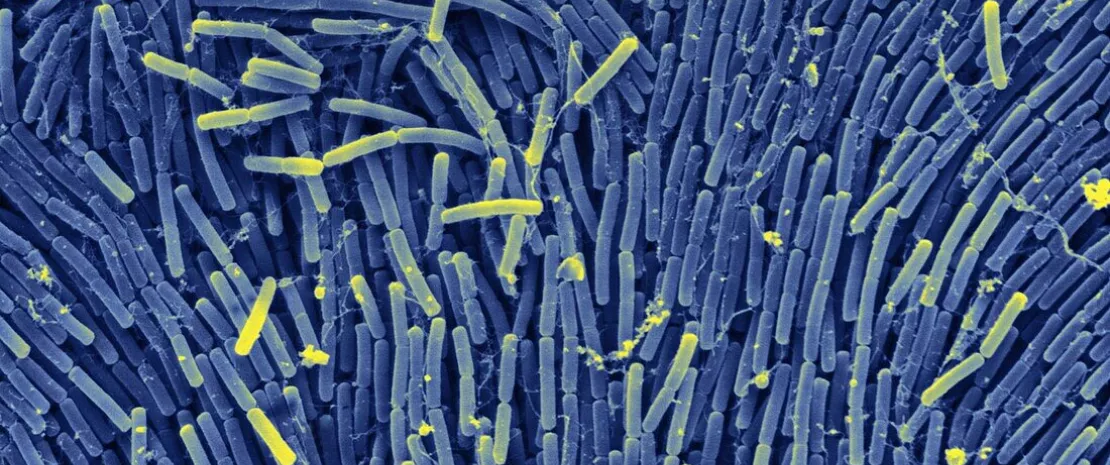
98% Proteobacteria, Firmicutes, Actinobacteria, and Bacteroidetes make up over 98% of the total gut microbiota in healthy individuals.
From dysbiosis to dyspepsia
The gastrointestinal tract hosts a microbiota that increases in abundance from the stomach (non-sterile) to the colon: Proteobacteria, Firmicutes, Actinobacteria, and Bacteroidetes account for over 98% of the gut microbiota in healthy individuals. This microbial community is widely implicated in digestive health, from preserving the integrity of the gut barrier to modulating the mucosal immune system.
At times, the balance of this community is upset, leading to dysbiosis: the presence of Helicobacter pylori in the stomach seems to contribute to the development and progression of FD, while a dysbiosis in the duodenum (an increase in Streptococcus, Firmicutes, Bacteroides, and Proteobacteria, together with a decrease in Prevotella, Veillonella, Leptotrichia, Actinomyces, Neisseria, and Porphyromonas) appears to correlate with FD.
40% Over 40% of patients worldwide suffer from functional gastrointestinal disorders, of which functional dyspepsia is one of the most common.
3% to 5% Functional dyspepsia accounts for 3% to 5% of visits to family doctors.
The gut microbiota may be involved both directly (an imbalance in composition and abundance may lead to gut dysfunction) and via the bacterial metabolites it produces, which can have a beneficial (e.g. short-chain fatty acids produced by Firmicutes) or harmful (pro-inflammatory sphingolipids produced by Bacteroidetes and Prevotellaceae) effect on the host.
2/3 Two-thirds of those affected by functional dyspepsia suffer from persistent, irregular symptoms that can affect their quality of life and even their psychological well-being.
8 times Patients with functional dyspepsia have an approximately eight-fold higher risk of irritable bowel syndrome than the general population.
Treatment via the gut microbiota
Modulation of the gut microbiota thus has widely recognized potential as a therapeutic approach. A number of clinical trials have underlined this potential: a combination of probiotic Bacillus strains (Bacillus coagulans, Bacillus clausii, and Bacillus subtilis) improves certain symptoms (belching, reflux, bloating), as does a probiotic combining Bacillus coagulans MY01 and Bacillus subtilis. A probiotic-enriched yogurt (Lactobacillus gasseri) did not alter patients’ symptoms but did reduce their frequency (17.3% vs. 35.2% in the placebo group).
Ultimately, a better understanding of the mechanisms involved may lead to more targeted diagnostic methods and treatments that focus on the gut microbiota and are just as effective.












