Gut microbiota signature for cirrhosis
What if a stool analysis, potentially supplemented by a blood test, were enough to diagnose liver cirrhosis and distinguish it from fibrosis? The following study suggests this may be possible.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
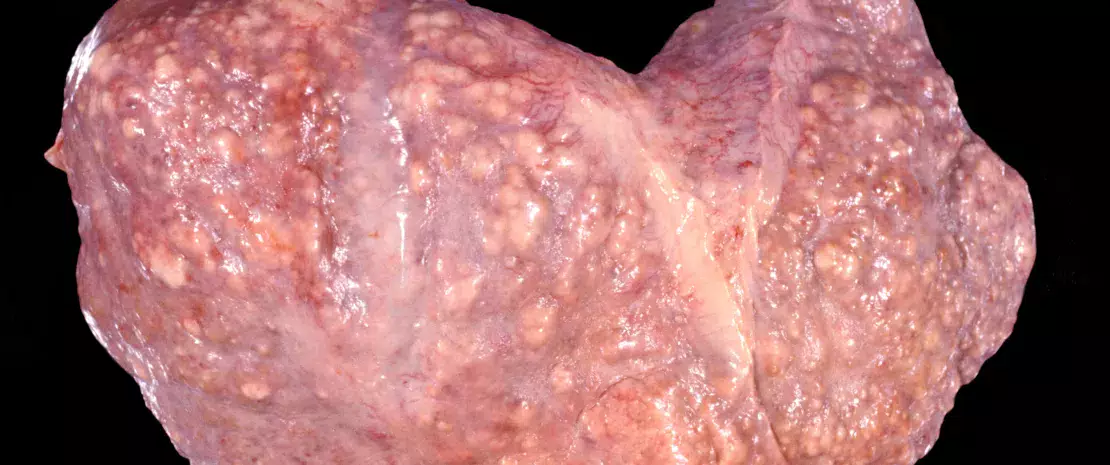
Non-alcoholic steatohepatitis (NASH) is thought to affect 24% of the world’s population and an alteration of the gut microbiota has been implicated in the progression from advanced fibrosis to cirrhosis. The stool microbiota of 163 US subjects was analyzed to determine the diagnostic capacity of this link. The participants included 54 non-NASH control subjects, 27 NASH patients suffering from cirrhosis (the most advanced stage of the disease) and their first-degree relatives. The results were supported by data from two independent Chinese and Italian cohorts.
Two independent signatures
The results showed a loss of bacterial diversity in the NASH-cirrhosis patients. This was found to be correlated with certain clinical parameters, notably LDL levels, coagulation, and blood insulin levels. More importantly, a (sidenote: Machine Learning Automatic learning whereby artificial intelligence solves a task based on metagenomic and metabolomic data collected, in this case the identification of discriminating bacterial species. Wazid M, Das AK, Chamola V, et al. Uniting cyber security and machine learning: Advantages, challenges and future research. ICT Express, 2022; 8(3), 313-321. ) approach identified a bacterial signature for cirrhosis based on 19 species with a diagnostic accuracy of 0.91. This dysbiosis was associated with a functional signature, notably the biosynthesis of specific amino acids (aromatic and branched), fatty acids and nucleotides. These results, which were confirmed in independent cohorts, suggest that the dysregulation of essential microbial metabolic processes may contribute to the progression of the disease to cirrhosis. Therefore, altered metabolite production may explain how gut dysbiosis can affect the liver. To further support this potential causal link, an independent signature based on 17 metabolites was identified, which provided the same diagnostic accuracy as the microbial signature. Significant correlations were found between the two signatures.
Distinguishing cirrhosis from fibrosis
The researchers subsequently sought to refine this microbial signature. By also considering age and blood albumin levels, they slightly improved the signature’s precision in distinguishing cirrhosis patients from control subjects, and above all validated its effectiveness in the Chinese and Italian cohorts. Lastly, the inclusion of a highly discriminating additional parameter (increased levels of aspartate aminotransferase (AST) in the blood of cirrhosis patients) has made it possible to distinguish cirrhosis from early-stage mild to moderate fibrosis.
A non-invasive diagnostic tool or even a treatment?
The robustness of this intestinal signature across geographically and culturally distinct populations shows its potential as a diagnostic tool for cirrhosis. Some bacterial species in the gut microbiota may become a useful non-invasive and universal diagnostic tool, or even potential targets for new therapeutic approaches.








