Cervicovaginal microbiota: a marker for persistent papillomavirus infection?
A recent study has shown that certain bacteria are associated with persistent HPV infection and that immunosuppressive factors may be involved in the host-pathogen interaction within the cervicovaginal microenvironment.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
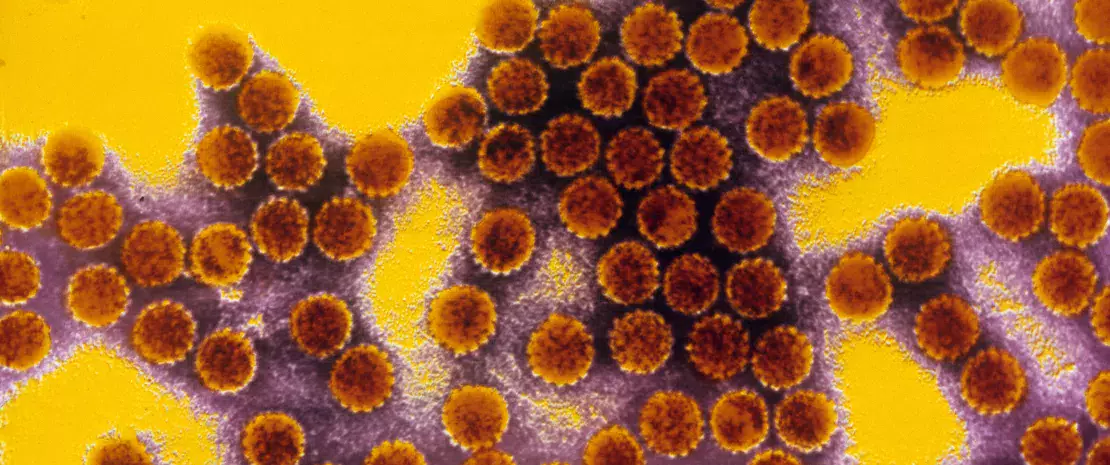
Persistent infection with high-risk human papillomavirus (HPV) is a leading cause of cervical dysplasia and cervical cancer. In recent years, numerous studies have suggested that a dysbiosis of the cervicovaginal microbiota may be closely related to persistent HPV infection, altered local immunity, and cervical intraepithelial neoplasia. A new study confirms this hypothesis.
Microbial signature of persistent HPV infection
In this new study, the cervicovaginal microbiota of 15 women was analyzed via 16S rRNA gene sequencing, and HPV genotyping was performed. Six of the women showed persistent infection (infection with the same HPV type for more than 12 months), four showed transient infection (infection cleared in less than 12 months) and five were HPV-negative. The three groups showed significant differences in the composition of the cervicovaginal microbiota. In the healthy women and those with transient infection, the Lactobacillus genus predominated, whereas women with persistent infection had a more diverse cervicovaginal microbiota. A statistical analysis revealed 36 bacteria to be associated with transient or persistent infection status, with these bacteria having the potential to serve as biomarkers. Among them, and in line with previous studies, the genera Acinetobacter, Prevotella and Pseudomonas were correlated with persistent infection. On the other hand, Lactobacillus iners was correlated with transient infection.
An increase in immunosuppressive cells
The women with persistent HPV infection had significantly higher concentrations of IL-6 and TNF-α in their cervical secretions and a higher number of regulatory T cells and myeloid-derived suppressor cells in their peripheral blood. Cervicovaginal dysbiosis may therefore create an inflammatory microenvironment, leading to an accumulation of immunosuppressive cells, which may in turn lead to the development of cancer.
Towards earlier diagnosis
The results of this study suggest that changes in the cervicovaginal microbiota may be linked to persistent HPV infection. However, it is not known whether dysbiosis induces persistence of the infection or vice versa. Despite this, the identification of a microbial signature for persistent HPV infection may allow earlier diagnosis, ultimately leading to earlier intervention to eradicate the infection and reduce the likelihood of developing malignant cervical lesions.









