When travel breeds antibiotic resistance
Be on alert if your patients are planning a trip abroad: such trips are associated with intestinal dysbiosis in 61% of American travelers, and the acquisition of antibiotic resistance in 38% of those travelers. We need to raise awareness of hygiene practices and of the countries where the risk is greatest.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
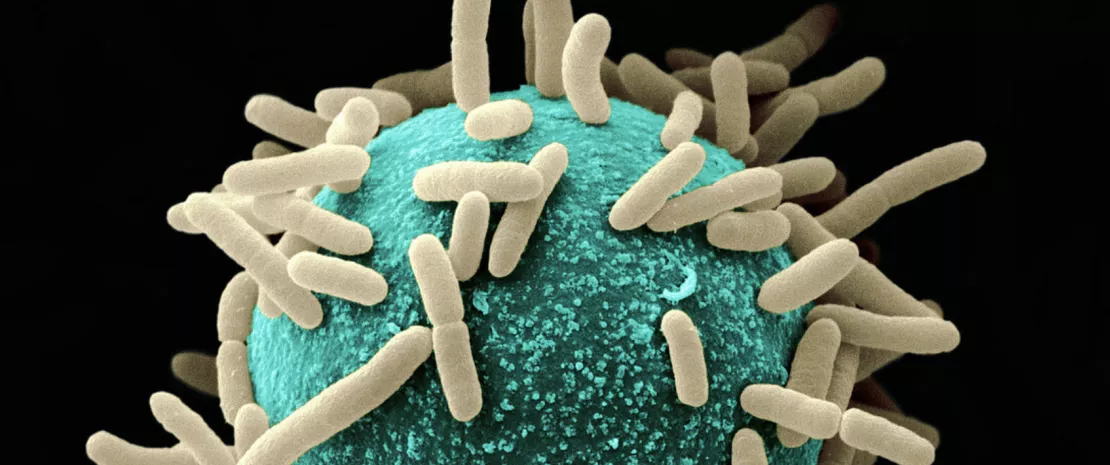
This is one of the downsides of international travel: among other things, it encourages the spread of antibiotic resistance. As knowledge on the subject is still very patchy (studies on small cohorts, poorly characterized microorganisms, etc.) despite the threat posed by such resistance, a team has screened the microbiota of 267 Americans recruited in 3 clinics (Boston, New York and Salt Lake City) before and after a trip abroad.
5 million deaths worldwide
In the United States, (sidenote: Antimicrobials Antimicrobials — such as antibiotics, antivirals, antifungals and antiparasitics — are drugs used to prevent and treat infections in humans, animals and plants. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance ) -resistant organisms are associated with over 2.8 million infections and 35,000 deaths per year. In 2019, it was estimated that nearly 5 million deaths worldwide were associated with antibiotic resistance, including 1.27 million deaths directly caused by it. 1
Dysbiosis in travelers
The first finding of the study is that travel disrupts the intestinal microbiota, with a significant loss of microbial diversity in 61% of travelers, varying according to destination (from 42% of travelers to Central America to 76% of those who went to South America).
The abundance of Escherichia spp. and several other enterobacteria (Klebsiella, Enterobacter and Salmonella) increases with the acquisition of new strains, while the genus Alistipes virtually disappears. Travel to South Asia increases the risk of returning with an intestinal stowaway, while consumption of unfiltered tap water or prior vaccination against typhus seems to limit it.
When resistance travels
A third of the 267 travelers reported diarrhea and 18% of them were treated with antibiotics.
More significantly, on returning from their trip, 38% of the 267 travelers had acquired at least one of the 3 types of resistant bacteria targeted by this study: of these, 98% acquired
(sidenote:
Extended-spectrum beta-lactamase (ESBL) producing Enterobacteriaceae
Enterobacteria that produce enzymes (extended-spectrum lactamases) with the ability to hydrolyze and cause resistance to various types of newer antibiotics. Klebsiella pneumoniae and Escherichia coli are the main ones. ESBL-producing Enterobacteriaceae, which make up the majority of multi-resistant bacteria, are responsible for potentially severe infections and prescriptions for broad-spectrum antibiotics.
Sources :
Pitout JD, Laupland KB. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008 Mar;8(3):159-66. doi: 10.1016/S1473-3099(08)70041-0.
Et Vodovar D, Marcadé G, Raskine L et al. Entérobactéries productrices de bêta-lactamases à spectre élargi : épidémiologie, facteurs de risque et mesures de prévention [Enterobacteriaceae producing extended spectrum beta-lactamase: epidemiology, risk factors, and prevention]. La Revue de medecine interne, 34(11), 687–693. https://doi.org/10.1016/j.revmed.2012.10.365
)
(in 98% of cases, E. coli), 18% colistin-resistant Enterobacteriaceae, and 3% carbapenemase-producing Enterobacteriaceae.
And which risk factors encourage the acquisition of such resistance? Visits to friends and relatives, a trip to South Asia and eating raw vegetables. On the other hand, pre-departure intestinal diversity, the presence of a specific bacterial taxon, street food consumption and antibiotic use did not change the situation.
One of the top 10 public health threats
WHO has declared that AMR is one of the top 10 public health threats facing humanity. 2
Limiting risks
Among the types of resistance acquired during travel, fluoroquinolone resistance was particularly noteworthy: more than 1 in 2 travelers (56%) without resistance before the trip returned with at least one gene associated with resistance to an antibiotic in this class. In all, the group of 267 travelers returned to the United States with 72 new resistance genes, 15 of which are of public health concern!
These results call for warnings (especially for the riskiest destinations) and a reminder of good practices (cooked vegetables, hand-washing, etc.). Conversely, modulating intestinal microbiota before the trip (with probiotics, for example) would have no added value in this particular case.
World AMR Awareness Week
World AMR Awareness Week (WAAW) is celebrated every year from November 18 to 24. In 2023, the theme chosen was “Preventing antimicrobial resistance together,” as in 2022. In fact, this resistance represents a threat not only to human beings, but also to animals, plants and the environment.
The aim of this campaign is to raise awareness of antimicrobial resistance and promote best practices, based on the "One Health" concept, among all stakeholders (the general public, doctors, veterinarians, breeders and farmers, decision-makers, etc.) in order to reduce the emergence and spread of resistant infections.







